test test
What Is So Fascinating About Marijuana News?
The Meaning of Marijuana News
If you’re against using Cannabis as you do not need to smoke you’re misinformed. As there is barely any cannabis left in a roach, some people today argue that the song is all about running out of cannabis and not having the ability to acquire high, exactly like the roach isn’t able to walk because it’s missing a leg. If you’re thinking about consuming cannabis please consult your health care provider first. Before visiting test.com the list, it’s important to be aware of the scientific reason cannabis works as a medication generally, and more specifically, the scientific reason it can send cancer into remission. At the moment, Medical Cannabis was still being used to take care of several health-related problems. In modern society, it is just starting to receive the recognition it deserves when it comes to treating diseases such as Epilepsy.
In nearly all the nation, at the present time, marijuana is illegal. To comprehend what marijuana does to the brain first you’ve got to know the key chemicals in marijuana and the various strains. If you are a person who uses marijuana socially at the occasional party, then you likely do not have that much to be concerned about. If you’re a user of medicinal marijuana, your smartphone is possibly the very first place you start looking for your community dispensary or a health care provider. As an issue of fact, there are just a few types of marijuana that are psychoactive. Medical marijuana has entered the fast-lane and now in case you reside in Arizona you can purchase your weed without leaving your vehicle. Medical marijuana has numerous therapeutic effects which will need to be dealt with and not only the so-called addictive qualities.
If you’re using marijuana for recreational purposes begin with a strain with a minimal dose of THC and see the way your body reacts. Marijuana is simpler to understand because it is both criminalized and decriminalized, based on the place you go in the nation. If a person is afflicted by chronic depression marijuana can directly affect the Amygdala that is accountable for your emotions.

Much enjoy the wine industry was just two or three decades past, the cannabis business has an image problem that’s keeping people away. In the event you want to learn where you are able to find marijuana wholesale companies near you, the very best place to seek out such companies is our site, Weed Finder. With the cannabis industry growing exponentially, and as more states start to legalize, individuals are beginning to learn that there is far more to cannabis than simply a plant that you smoke. In different states, the work of legal marijuana has produced a patchwork of banking and tax practices. Then the marijuana sector is ideal for you.
Marijuana News for Dummies
Know what medical cannabis options can be found in your state and the way they respond to your qualifying medical condition. They can provide medicinal benefits, psychotropic benefits, and any combination of both, and being able to articulate what your daily responsibilities are may help you and your physician make informed, responsible decisions regarding the options that are appropriate for you, thus protecting your employment, your family and yourself from untoward events. In the modern society, using drugs has become so prevalent it has come to be a component of normal life, irrespective of age or gender. Using marijuana in the USA is growing at a quick rate.
Berikut 7 Barang Antik Belanda Bernilai Harga Jual Tinggi – Barang antik adalah benda atau koleksi yang memiliki usia tua, umumnya lebih dari 100 tahun, dan memiliki nilai estetika, sejarah, atau keunikan tertentu. Barang-barang ini sering kali menjadi bukti dari masa lampau, dan sering kali dicari oleh kolektor, penggemar, atau individu yang menghargai nilai-nilai kultural dan sejarah. Barang antik bisa beragam, mulai dari perabotan, perhiasan, seni, keramik, buku, hingga peralatan rumah tangga. Barang-barang tersebut sering kali memiliki ciri khas atau keunikan dalam desain, bahan, atau pembuatannya yang mencerminkan periode waktu tertentu dalam sejarah.
Kesimpulan dari barang antik adalah bahwa mereka memiliki nilai yang lebih dari sekadar benda fisik. Barang-barang ini sering dianggap berharga karena usianya yang tua, keunikan desain, kualitas kerja yang superior, atau hubungan dengan periode sejarah tertentu. Karena karakteristik ini, barang-barang antik sering dicari dan dihargai oleh kolektor, penggemar, dan individu yang ingin memiliki bagian dari warisan kultural dan sejarah. Penting untuk memahami nilai dan karakteristik unik dari barang antik sebelum membeli atau menjualnya untuk menghindari penilaian yang salah.
Sebagai negara dengan sejarah yang kaya, Belanda memiliki sejumlah barang antik yang memiliki nilai jual yang tinggi di pasar kolektor. Berikut adalah beberapa contoh barang antik dari Belanda yang sering dicari dan memiliki harga jual tinggi:

Lukisan Klasik Belanda
Lukisan-lukisan dari seniman-seniman Belanda terkenal seperti Rembrandt, Vermeer, atau Van Gogh adalah karya seni yang sangat berharga dan dapat memiliki nilai jual yang sangat tinggi di pasar seni antik.
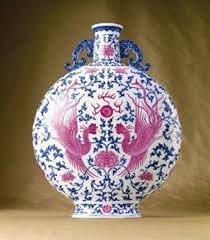
Porselen Delft
Porselen Delft, terkenal dengan dekorasi biru putihnya yang khas, adalah jenis kerajinan porselen dari Belanda yang sering memiliki nilai tinggi di pasar antik.
Kerajinan Kayu dan Ukiran
Kerajinan kayu khas Belanda seperti lemari, meja, jam, atau kerajinan ukiran kayu lainnya yang berasal dari masa lalu atau yang memiliki desain unik dan khas Belanda sering menjadi incaran kolektor antik.
Kerajinan Logam
Barang-barang logam antik seperti cangkir perak, perhiasan, atau barang-barang logam lainnya yang berasal dari periode klasik atau terkait dengan sejarah Belanda memiliki nilai jual yang tinggi.
Koin Kuno atau Uang Kertas
Koleksi koin atau uang kuno dari Belanda, terutama yang berasal dari masa lalu atau koin-koin langka dari era tertentu, sering dicari oleh kolektor numismatik.
Perabotan Klasik
Perabotan klasik Belanda seperti kursi, laci, atau perabotan lainnya dengan desain khas Belanda atau dari era tertentu sering memiliki nilai tinggi di pasar antik.
Barang-Barang Terkait Sejarah Kolonial
Barang-barang antik yang terkait dengan sejarah kolonial Belanda seperti peta kuno, artefak, atau barang-barang yang terkait dengan masa penjelajahan dan perdagangan dunia Belanda sering memiliki nilai jual yang tinggi.
Pastikan untuk mendapatkan penilaian dari ahli atau pelelang yang berpengalaman sebelum menjual barang-barang antik ini untuk mengetahui nilai sebenarnya dari barang-barang tersebut. Keaslian, usia, dan kondisi barang dapat sangat mempengaruhi nilai jualnya.
Berikut 7 Barang Antik Russia Bernilai Harga Jual Tinggi – Barang antik adalah benda atau koleksi yang memiliki usia tua, umumnya lebih dari 100 tahun, dan memiliki nilai estetika, sejarah, atau keunikan tertentu. Barang-barang ini sering kali menjadi bukti dari masa lampau, dan sering kali dicari oleh kolektor, penggemar, atau individu yang menghargai nilai-nilai kultural dan sejarah. Barang antik bisa beragam, mulai dari perabotan, perhiasan, seni, keramik, buku, hingga peralatan rumah tangga. Barang-barang tersebut sering kali memiliki ciri khas atau keunikan dalam desain, bahan, atau pembuatannya yang mencerminkan periode waktu tertentu dalam sejarah.
Kesimpulan dari barang antik adalah bahwa mereka memiliki nilai yang lebih dari sekadar benda fisik. Barang-barang ini sering dianggap berharga karena usianya yang tua, keunikan desain, kualitas kerja yang superior, atau hubungan dengan periode sejarah tertentu. Karena karakteristik ini, barang-barang antik sering dicari dan dihargai oleh kolektor, penggemar, dan individu yang ingin memiliki bagian dari warisan kultural dan sejarah. Penting untuk memahami nilai dan karakteristik unik dari barang antik sebelum membeli atau menjualnya untuk menghindari penilaian yang salah.
Beberapa barang antik dari Rusia memiliki nilai tinggi karena sejarah, kebudayaan, dan seni yang unik. Berikut adalah beberapa contoh barang antik dari Rusia yang sering dicari oleh kolektor dan memiliki harga jual tinggi:

Ikona Kuno
Ikona Rusia, yaitu lukisan-lukisan klasik berisi gambar suci atau tokoh-tokoh agama, sering memiliki nilai historis dan seni yang tinggi di pasar antik.
Fabergé Eggs (Telur Fabergé)
Telur Fabergé adalah karya seni perhiasan berharga yang diciptakan oleh House of Fabergé untuk para Tsar Rusia. Karya-karya ini sangat langka dan sering memiliki nilai jual yang sangat tinggi.
Kerajinan Porselen Rusia
Barang-barang porselen kuno dari produsen Rusia seperti Kuznetsov, Gardner, atau Lomonosov, terutama yang memiliki dekorasi istimewa atau yang terkait dengan keluarga kerajaan, sering dicari oleh kolektor.
Lukisan Klasik Rusia
Lukisan-lukisan klasik dari seniman Rusia terkenal seperti Ivan Aivazovsky, Kazimir Malevich, atau Ivan Shishkin dapat memiliki nilai seni dan sejarah yang tinggi.
Kerajinan Ukiran Kayu (Matryoshka)
Boneka Matryoshka atau boneka nesting doll tradisional Rusia yang diukir dari kayu sering menjadi simbol Rusia dan dapat memiliki nilai jual yang tinggi, terutama yang terbuat pada masa lalu atau oleh pengrajin terkenal.
Senjata Kuno Rusia
Senjata kuno Rusia seperti pedang, pisau, atau senjata tradisional lainnya yang terkait dengan sejarah Rusia atau periode kerajaan sering dicari oleh kolektor.
Uang Kuno atau Koin
Uang kuno Rusia, terutama dari era Tsarist atau koin-koin kuno dari zaman-zaman penting dalam sejarah Rusia, sering menjadi koleksi yang sangat dihargai.
Barang-barang antik Rusia ini sering memiliki nilai yang tinggi karena keunikan, sejarah, dan seni yang dimilikinya. Pastikan untuk mendapatkan penilaian dari ahli atau pelelang yang berpengalaman sebelum menjual barang-barang antik ini untuk mengetahui nilai sebenarnya dari barang-barang tersebut.
Berikut 7 Barang Antik Amerika Bernilai Harga Jual Tinggi – Barang antik adalah benda atau koleksi yang memiliki usia tua, umumnya lebih dari 100 tahun, dan memiliki nilai estetika, sejarah, atau keunikan tertentu. Barang-barang ini sering kali menjadi bukti dari masa lampau, dan sering kali dicari oleh kolektor, penggemar, atau individu yang menghargai nilai-nilai kultural dan sejarah. Barang antik bisa beragam, mulai dari perabotan, perhiasan, seni, keramik, buku, hingga peralatan rumah tangga. Barang-barang tersebut sering kali memiliki ciri khas atau keunikan dalam desain, bahan, atau pembuatannya yang mencerminkan periode waktu tertentu dalam sejarah.
Kesimpulan dari barang antik adalah bahwa mereka memiliki nilai yang lebih dari sekadar benda fisik. Barang-barang ini sering dianggap berharga karena usianya yang tua, keunikan desain, kualitas kerja yang superior, atau hubungan dengan periode sejarah tertentu. Karena karakteristik ini, barang-barang antik sering dicari dan dihargai oleh kolektor, penggemar, dan individu yang ingin memiliki bagian dari warisan kultural dan sejarah. Penting untuk memahami nilai dan karakteristik unik dari barang antik sebelum membeli atau menjualnya untuk menghindari penilaian yang salah.
Barang-barang antik Amerika sering dicari oleh kolektor dan penggemar barang-barang bersejarah. Berikut beberapa contoh barang antik dari Amerika yang memiliki nilai jual tinggi:

Peralatan Senjata Kuno
Senjata kuno Amerika seperti senapan, pistol, atau senjata api klasik lainnya dari era Revolusi Amerika, Perang Saudara, atau Perang Dunia II sering dicari oleh kolektor senjata dan dapat memiliki nilai yang tinggi.
Peralatan Budaya Asli Amerika
Artefak atau kerajinan tangan dari suku-suku asli Amerika seperti Hopi, Navajo, Sioux, atau suku-suku lainnya yang mencerminkan warisan budaya mereka, seperti kerajinan anyaman, senjata, atau barang-barang pemujaan, sering menjadi incaran kolektor.
Koin dan Uang Kuno
Koleksi koin atau uang kuno Amerika dari era kolonial, dollar emas, atau koin langka yang terkait dengan sejarah penting sering dicari oleh kolektor numismatik.
Porselen dan Barang Porselen Klasik
Porselen klasik Amerika dari produsen terkenal seperti Wedgwood, Davenport, atau porselen dari periode Victorian atau Edwardian sering memiliki nilai yang tinggi di pasar antik.
Lukisan dan Karya Seni
Lukisan-lukisan klasik Amerika, karya seni dari seniman terkenal seperti Norman Rockwell, Georgia O’Keeffe, atau karya seni kontemporer Amerika lainnya dapat memiliki nilai jual yang tinggi di pasar seni.
Koleksi Perabotan
Perabotan antik Amerika, seperti meja, kursi, lemari, atau perabotan khas era Victorian, kolonial, atau perabotan yang terkait dengan sejarah penting sering dicari oleh penggemar perabotan antik.
Barang-barang Terkait Presiden atau Politisi Penting
Barang-barang terkait dengan presiden Amerika atau tokoh-tokoh politik penting, seperti surat-surat asli, tanda tangan, atau barang-barang milik mereka, sering memiliki nilai yang tinggi.
Pastikan untuk mendapatkan penilaian yang akurat dari ahli atau pelelang yang berpengalaman sebelum menjual barang-barang antik ini karena keaslian, kondisi, dan sejarah barang dapat mempengaruhi nilai jualnya.
Berikut 7 Barang Antik Jepang Bernilai Harga Jual Tinggi – Barang antik adalah benda atau koleksi yang memiliki usia tua, umumnya lebih dari 100 tahun, dan memiliki nilai estetika, sejarah, atau keunikan tertentu. Barang-barang ini sering kali menjadi bukti dari masa lampau, dan sering kali dicari oleh kolektor, penggemar, atau individu yang menghargai nilai-nilai kultural dan sejarah. Barang antik bisa beragam, mulai dari perabotan, perhiasan, seni, keramik, buku, hingga peralatan rumah tangga. Barang-barang tersebut sering kali memiliki ciri khas atau keunikan dalam desain, bahan, atau pembuatannya yang mencerminkan periode waktu tertentu dalam sejarah.
Kesimpulan dari barang antik adalah bahwa mereka memiliki nilai yang lebih dari sekadar benda fisik. Barang-barang ini sering dianggap berharga karena usianya yang tua, keunikan desain, kualitas kerja yang superior, atau hubungan dengan periode sejarah tertentu. Karena karakteristik ini, barang-barang antik sering dicari dan dihargai oleh kolektor, penggemar, dan individu yang ingin memiliki bagian dari warisan kultural dan sejarah. Penting untuk memahami nilai dan karakteristik unik dari barang antik sebelum membeli atau menjualnya untuk menghindari penilaian yang salah.
Barang-barang antik Jepang sering kali memiliki nilai tinggi karena keindahan, keunikan, dan warisan budayanya. Berikut adalah beberapa contoh barang antik Jepang yang dapat memiliki harga jual yang tinggi:

Keramik Kuno (Yakimono)
Porselen, tembikar, atau barang-barang keramik Jepang kuno seperti Imari, Kutani, atau Hagi ware sering dicari oleh kolektor karena keindahan dan sejarahnya.
Pedang Samurai (Katana)
Pedang Samurai atau katana adalah senjata khas Jepang yang terkenal dengan keindahan, kehebatan pembuatan, dan nilai sejarahnya. Pedang-pedang kuno dari periode Samurai sering memiliki harga yang sangat tinggi di pasar antik.
Lukisan dan Karya Seni Tradisional
Lukisan-lukisan klasik, kaligrafi, ukiran kayu, atau seni tradisional Jepang lainnya seperti Ukiyo-e (lukisan kayu bergaya Edo) atau karya seni dari seniman terkenal sering memiliki nilai jual yang tinggi di pasar seni antik.
Kain Kimono
Kimono kuno yang terbuat dari bahan khusus, dihiasi dengan pola tradisional yang rumit dan khas, atau kimono yang terkait dengan sejarah penting sering menjadi koleksi para penggemar mode atau budaya Jepang.
Uang Kuno atau Koin
Koleksi uang kuno Jepang dari era Kuno hingga zaman modern, termasuk koin-koin langka atau uang-uang kuno yang terkait dengan era tertentu, sering dicari oleh kolektor numismatik.
Lacquerware (Barang dari Lak)
Barang-barang yang terbuat dari lak, seperti laci, kotak, atau perabotan yang dihiasi dengan teknik lapisan lak Jepang yang tradisional, sering menjadi incaran penggemar barang antik.
Porselen dan Figur Kecil (Netsuke)
Porselen kuno, figur, atau netsuke yang digunakan sebagai hiasan atau aksesoris pada masa lalu sering memiliki nilai tinggi di pasar antik.
Barang-barang antik Jepang ini sering kali memiliki nilai yang tinggi karena keunikan budaya Jepang yang unik dan indah. Namun, pastikan untuk mendapatkan penilaian yang akurat dari ahli atau pelelang yang berpengalaman sebelum menjual barang-barang antik ini.
Berikut 7 Barang Antik Malaysia Bernilai Harga Jual Tinggi – Barang antik adalah benda atau koleksi yang memiliki usia tua, umumnya lebih dari 100 tahun, dan memiliki nilai estetika, sejarah, atau keunikan tertentu. Barang-barang ini sering kali menjadi bukti dari masa lampau, dan sering kali dicari oleh kolektor, penggemar, atau individu yang menghargai nilai-nilai kultural dan sejarah. Barang antik bisa beragam, mulai dari perabotan, perhiasan, seni, keramik, buku, hingga peralatan rumah tangga. Barang-barang tersebut sering kali memiliki ciri khas atau keunikan dalam desain, bahan, atau pembuatannya yang mencerminkan periode waktu tertentu dalam sejarah.
Kesimpulan dari barang antik adalah bahwa mereka memiliki nilai yang lebih dari sekadar benda fisik. Barang-barang ini sering dianggap berharga karena usianya yang tua, keunikan desain, kualitas kerja yang superior, atau hubungan dengan periode sejarah tertentu. Karena karakteristik ini, barang-barang antik sering dicari dan dihargai oleh kolektor, penggemar, dan individu yang ingin memiliki bagian dari warisan kultural dan sejarah. Penting untuk memahami nilai dan karakteristik unik dari barang antik sebelum membeli atau menjualnya untuk menghindari penilaian yang salah.
Barang-barang antik yang bernilai tinggi di Malaysia sering kali terkait dengan warisan budaya dan sejarah yang khas dari negara tersebut. Berikut adalah beberapa barang antik Malaysia yang bisa memiliki harga jual tinggi:

Kerajinan Perak
Malaysia terkenal dengan kerajinan peraknya. Barang-barang seperti perhiasan, cincin, gelang, atau patung perak kuno sering dicari oleh kolektor atau penggemar barang antik dan bisa memiliki harga jual yang tinggi.
Kain Songket
Songket adalah kain tenun tradisional yang dihiasi dengan benang emas atau perak. Songket kuno yang langka atau memiliki pola yang unik sering memiliki nilai jual yang tinggi.
Senjata Tradisional
Seperti halnya di Indonesia, senjata tradisional seperti keris, kris, atau senjata tradisional Melayu lainnya yang langka atau memiliki sejarah yang terkait dengan tokoh-tokoh penting bisa memiliki nilai jual yang tinggi.
Uang Kuno
Koleksi uang kuno Malaysia, terutama dari zaman kolonial Inggris atau uang-uang tradisional Melayu, sering menjadi incaran para kolektor uang kuno.
Piring atau Kerajinan Porselen
Barang-barang porselen tua, piring kuno, atau kerajinan porselen tradisional Malaysia bisa memiliki nilai yang tinggi di pasar antik.
Lukisan Tradisional atau Klasik
Lukisan-lukisan tradisional atau klasik Malaysia, terutama dari seniman ternama atau dari periode zaman dahulu, sering memiliki nilai seni yang tinggi dan menjadi koleksi para penggemar seni.
Wayang Kulit atau Seni Pertunjukan Tradisional
Barang-barang terkait dengan seni pertunjukan tradisional seperti wayang kulit atau peralatan pertunjukan tradisional lainnya bisa menjadi incaran kolektor seni dan memiliki nilai yang tinggi.
Seperti halnya dalam menjual barang-barang antik Indonesia, pastikan untuk mendapatkan penilaian dari ahli atau pelelang yang berpengalaman untuk mengetahui nilai sebenarnya dari barang-barang antik ini sebelum menjualnya.
Berikut 7 Barang Antik Indonesia Bernilai Harga Jual Tinggi – Barang antik adalah benda atau koleksi yang memiliki usia tua, umumnya lebih dari 100 tahun, dan memiliki nilai estetika, sejarah, atau keunikan tertentu. Barang-barang ini sering kali menjadi bukti dari masa lampau, dan sering kali dicari oleh kolektor, penggemar, atau individu yang menghargai nilai-nilai kultural dan sejarah. Barang antik bisa beragam, mulai dari perabotan, perhiasan, seni, keramik, buku, hingga peralatan rumah tangga. Barang-barang tersebut sering kali memiliki ciri khas atau keunikan dalam desain, bahan, atau pembuatannya yang mencerminkan periode waktu tertentu dalam sejarah.
Kesimpulan dari barang antik adalah bahwa mereka memiliki nilai yang lebih dari sekadar benda fisik. Barang-barang ini sering dianggap berharga karena usianya yang tua, keunikan desain, kualitas kerja yang superior, atau hubungan dengan periode sejarah tertentu. Karena karakteristik ini, barang-barang antik sering dicari dan dihargai oleh kolektor, penggemar, dan individu yang ingin memiliki bagian dari warisan kultural dan sejarah. Penting untuk memahami nilai dan karakteristik unik dari barang antik sebelum membeli atau menjualnya untuk menghindari penilaian yang salah.
Beberapa barang antik Indonesia memiliki nilai jual yang tinggi karena keunikan, sejarah, dan keaslian mereka. Beberapa dari barang-barang antik ini termasuk:

Keris
Keris adalah senjata tradisional Indonesia yang memiliki nilai historis dan seni yang tinggi. Keris yang langka, memiliki pamor yang unik, atau memiliki sejarah terkait tokoh penting sering memiliki harga jual yang tinggi.
Wayang Kulit
Wayang kulit adalah seni tradisional Indonesia yang terkenal. Beberapa figur wayang kulit yang langka, dibuat oleh dalang ternama, atau memiliki usia yang tua bisa memiliki nilai tinggi di pasar antik.
Uang Kuno
Uang kuno Indonesia, khususnya uang-uang dari masa lalu yang langka atau koleksi uang kertas atau logam dari era kolonial atau zaman kerajaan, sering dicari oleh kolektor.
Kain Batik Kuno
Batik adalah warisan budaya Indonesia yang sangat dihargai. Kain batik kuno dengan pola yang langka, proses pembuatan yang tradisional, dan umur yang tua memiliki nilai jual yang tinggi di pasar antik.
Kerajinan Perak atau Perunggu
Barang-barang seperti arca perunggu, perhiasan perak kuno, atau patung yang terbuat dari logam mulia sering dicari oleh kolektor dan memiliki nilai jual yang tinggi.
Senjata Tradisional Lainnya
Selain keris, senjata tradisional lain seperti tombak, pedang, atau senjata tradisional suku-suku di Indonesia yang memiliki nilai historis dan seni tinggi dapat memiliki harga jual yang tinggi di pasar antik.
Lukisan Klasik Indonesia
Lukisan klasik dari pelukis ternama Indonesia, terutama dari periode lukisan klasik Indonesia pada abad ke-19 dan ke-20, memiliki nilai seni yang tinggi dan bisa memiliki harga jual yang fantastis di pasar seni antik.
Pastikan untuk mendapatkan penilaian yang akurat dari ahli atau pelelang yang berpengalaman sebelum menjual barang-barang antik ini, karena keaslian, usia, dan kondisi barang sangat mempengaruhi nilai jual mereka.
7 Barang Koleksi yang Jadi Incaran Wisatawan Saat Pelesir – Barang antik adalah benda atau koleksi yang memiliki usia tua, umumnya lebih dari 100 tahun, dan memiliki nilai estetika, sejarah, atau keunikan tertentu. Barang-barang ini sering kali menjadi bukti dari masa lampau, dan sering kali dicari oleh kolektor, penggemar, atau individu yang menghargai nilai-nilai kultural dan sejarah. Barang antik bisa beragam, mulai dari perabotan, perhiasan, seni, keramik, buku, hingga peralatan rumah tangga. Barang-barang tersebut sering kali memiliki ciri khas atau keunikan dalam desain, bahan, atau pembuatannya yang mencerminkan periode waktu tertentu dalam sejarah.
Kesimpulan dari barang antik adalah bahwa mereka memiliki nilai yang lebih dari sekadar benda fisik. Barang-barang ini sering dianggap berharga karena usianya yang tua, keunikan desain, kualitas kerja yang superior, atau hubungan dengan periode sejarah tertentu. Karena karakteristik ini, barang-barang antik sering dicari dan dihargai oleh kolektor, penggemar, dan individu yang ingin memiliki bagian dari warisan kultural dan sejarah. Penting untuk memahami nilai dan karakteristik unik dari barang antik sebelum membeli atau menjualnya untuk menghindari penilaian yang salah.
Wisatawan seringkali tertarik untuk mengoleksi atau membeli berbagai barang khas atau suvenir yang terkait dengan destinasi wisata yang mereka kunjungi. Berikut adalah tujuh jenis barang koleksi yang sering menjadi incaran wisatawan saat berlibur:

Suvenir Lokal atau Cendera Mata
Barang-barang kecil seperti magnet kulkas, gantungan kunci, topi, kaos, atau gantungan tas dengan desain dan logo yang mencirikan tempat wisata tersebut.
Karya Seni Lokal
Lukisan, ukiran, patung, atau kerajinan tangan lokal yang menggambarkan budaya, seni, atau keunikan tempat wisata yang dikunjungi.
Produk Kuliner Khas
Makanan atau produk makanan khas daerah yang bisa dibawa pulang, seperti bumbu masakan, makanan ringan, atau kopi lokal.
Pakaian Tradisional
Pakaian tradisional atau aksesori khas daerah seperti kain batik, sarung, pakaian etnik, atau syal yang dianggap sebagai benda eksotis dari tempat tersebut.
Koleksi Kerajinan Tangan
Barang-barang yang terbuat dari bahan lokal seperti keramik, tenunan, anyaman, atau perhiasan yang unik dan khas dari daerah tersebut.
Buku atau Materi Literatur
Buku-buku sejarah lokal, cerita rakyat, buku panduan, atau literatur tentang kebudayaan dan sejarah daerah yang dikunjungi.
Oleh-oleh Khas
Produk-produk unik atau tradisional yang spesifik untuk destinasi, seperti minuman khas, hasil pertanian, atau produk-produk alam yang hanya ditemukan di daerah tersebut.
Pilihan barang koleksi atau suvenir bisa berbeda-beda tergantung pada minat dan preferensi wisatawan serta ketersediaan produk yang ditawarkan di tempat tujuan wisata tersebut. Yang penting adalah, barang-barang ini menjadi kenangan yang menyenangkan dari perjalanan wisata dan dapat mengingatkan wisatawan akan pengalaman yang mereka alami.
4 Penemuan Barang Antik dan Kuno Pembuka Tabir Peradaban Dunia – Barang antik adalah benda atau koleksi yang memiliki usia tua, umumnya lebih dari 100 tahun, dan memiliki nilai estetika, sejarah, atau keunikan tertentu. Barang-barang ini sering kali menjadi bukti dari masa lampau, dan sering kali dicari oleh kolektor, penggemar, atau individu yang menghargai nilai-nilai kultural dan sejarah. Barang antik bisa beragam, mulai dari perabotan, perhiasan, seni, keramik, buku, hingga peralatan rumah tangga. Barang-barang tersebut sering kali memiliki ciri khas atau keunikan dalam desain, bahan, atau pembuatannya yang mencerminkan periode waktu tertentu dalam sejarah.
Kesimpulan dari barang antik adalah bahwa mereka memiliki nilai yang lebih dari sekadar benda fisik. Barang-barang ini sering dianggap berharga karena usianya yang tua, keunikan desain, kualitas kerja yang superior, atau hubungan dengan periode sejarah tertentu. Karena karakteristik ini, barang-barang antik sering dicari dan dihargai oleh kolektor, penggemar, dan individu yang ingin memiliki bagian dari warisan kultural dan sejarah. Penting untuk memahami nilai dan karakteristik unik dari barang antik sebelum membeli atau menjualnya untuk menghindari penilaian yang salah.
Penemuan barang-barang antik dan kuno telah memainkan peran penting dalam membuka tabir peradaban dunia, memberikan wawasan yang mendalam tentang sejarah manusia. Berikut adalah empat penemuan barang antik yang penting dalam mengungkap sejarah peradaban dunia:

Pompeii dan Herculaneum (Italia)
Penemuan kota-kota Romawi kuno ini, yang tertimbun oleh letusan gunung Vesuvius pada tahun 79 Masehi, memberikan pemahaman yang mendalam tentang kehidupan dan budaya Romawi pada masa itu. Artefak yang ditemukan di situs-situs ini seperti patung, lukisan, dan benda-benda sehari-hari telah memberikan gambaran yang jelas tentang kehidupan kuno.
Kuil Mesir Kuno di Karnak dan Luxor
Sisa-sisa kuil-kuil megah di Karnak dan Luxor di Mesir memberikan wawasan tentang kehidupan dan keagamaan orang Mesir kuno. Dinding-dinding yang dihiasi dengan relief dan hieroglif memberikan pengetahuan tentang kebudayaan, kepercayaan, dan kegiatan keagamaan mereka.
Tutankhamun’s Tomb (Lembah Para Raja, Mesir)
Penemuan makam Firaun Tutankhamun pada tahun 1922 oleh Howard Carter menjadi salah satu penemuan arkeologi terbesar dalam sejarah. Isi makam termasuk harta karun dan barang-barang yang berharga, memberikan informasi yang berharga tentang seni, budaya, dan kehidupan sehari-hari di Mesir kuno.
Sitara Mohenjo-Daro (Pakistan)
Mohenjo-Daro, salah satu situs peradaban lembah Indus, mengungkapkan sejumlah temuan yang memberikan wawasan tentang kehidupan peradaban Indus kuno. Sitara (lubang kancing berhias) dan benda-benda lainnya memberikan gambaran tentang kemajuan teknologi, sistem sanitasi, dan organisasi sosial mereka.
Penemuan-penemuan ini, bersama dengan banyak penemuan arkeologi lainnya, telah menjadi kunci dalam memahami perjalanan peradaban manusia. Barang-barang antik ini memberikan kita wawasan yang berharga tentang budaya, agama, teknologi, dan kehidupan sehari-hari manusia di masa lalu.
9 Barang Antik Termahal di Dunia, Capai Triliunan Rupiah – Barang antik adalah benda atau koleksi yang memiliki usia tua, umumnya lebih dari 100 tahun, dan memiliki nilai estetika, sejarah, atau keunikan tertentu. Barang-barang ini sering kali menjadi bukti dari masa lampau, dan sering kali dicari oleh kolektor, penggemar, atau individu yang menghargai nilai-nilai kultural dan sejarah. Barang antik bisa beragam, mulai dari perabotan, perhiasan, seni, keramik, buku, hingga peralatan rumah tangga. Barang-barang tersebut sering kali memiliki ciri khas atau keunikan dalam desain, bahan, atau pembuatannya yang mencerminkan periode waktu tertentu dalam sejarah.
Kesimpulan dari barang antik adalah bahwa mereka memiliki nilai yang lebih dari sekadar benda fisik. Barang-barang ini sering dianggap berharga karena usianya yang tua, keunikan desain, kualitas kerja yang superior, atau hubungan dengan periode sejarah tertentu. Karena karakteristik ini, barang-barang antik sering dicari dan dihargai oleh kolektor, penggemar, dan individu yang ingin memiliki bagian dari warisan kultural dan sejarah. Penting untuk memahami nilai dan karakteristik unik dari barang antik sebelum membeli atau menjualnya untuk menghindari penilaian yang salah.
Beberapa barang antik yang dihargai tinggi di pasar antik internasional antara lain:

Piala Ratu Artemis
Salah satu mangkuk porselen Cina kuno dari Dinasti Ming yang terjual seharga jutaan dolar karena keunikan desain dan asal-usulnya yang langka.
Vase Porcelain Qing Dynasty
Sebuah vas porselen kuno dari Dinasti Qing China yang dijual dengan harga tinggi karena kualitasnya yang unik dan kondisi yang sangat baik.
Piala Warwick
Artefak abad ke-18 yang terbuat dari perak sterling yang memiliki nilai sejarah yang tinggi, terjual dengan harga fantastis dalam lelang.
Lukisan “Salvator Mundi” oleh Leonardo da Vinci
Lukisan ini dianggap sebagai salah satu karya terbesar dari Leonardo da Vinci yang telah terjual dengan harga yang luar biasa tinggi dalam lelang seni.
Batang Korma 2.000 Tahun
Batang korma kuno yang berasal dari Dinasti Han di Tiongkok yang dianggap sebagai artefak langka dan berharga tinggi di pasar antik.
Piring Porselen Dinasti Ming
Piring-piring porselen kuno dari Dinasti Ming yang memiliki nilai sejarah dan seni yang tinggi, terkadang terjual dengan harga yang mencapai jutaan dolar.
Informasi mengenai harga barang antik yang sangat tinggi dapat berubah seiring waktu, tergantung pada permintaan pasar, keunikan, kondisi barang, dan kisah di balik setiap artefak tersebut.
Berikut 5 Cara Jual Barang Antik, Bisa Untung Besar! – Barang antik adalah benda atau koleksi yang memiliki usia tua, umumnya lebih dari 100 tahun, dan memiliki nilai estetika, sejarah, atau keunikan tertentu. Barang-barang ini sering kali menjadi bukti dari masa lampau, dan sering kali dicari oleh kolektor, penggemar, atau individu yang menghargai nilai-nilai kultural dan sejarah. Barang antik bisa beragam, mulai dari perabotan, perhiasan, seni, keramik, buku, hingga peralatan rumah tangga. Barang-barang tersebut sering kali memiliki ciri khas atau keunikan dalam desain, bahan, atau pembuatannya yang mencerminkan periode waktu tertentu dalam sejarah.
Kesimpulan dari barang antik adalah bahwa mereka memiliki nilai yang lebih dari sekadar benda fisik. Barang-barang ini sering dianggap berharga karena usianya yang tua, keunikan desain, kualitas kerja yang superior, atau hubungan dengan periode sejarah tertentu. Karena karakteristik ini, barang-barang antik sering dicari dan dihargai oleh kolektor, penggemar, dan individu yang ingin memiliki bagian dari warisan kultural dan sejarah. Penting untuk memahami nilai dan karakteristik unik dari barang antik sebelum membeli atau menjualnya untuk menghindari penilaian yang salah.
Berikut adalah beberapa cara untuk menjual barang antik dengan potensi mendapatkan keuntungan yang lebih besar:

Mengetahui Nilai Barang Antik Anda
Langkah pertama yang penting adalah mengetahui nilai sebenarnya dari barang antik yang Anda miliki. Carilah informasi tentang barang-barang tersebut, baik melalui penelitian online, konsultan antik, atau ahli penilaian yang dapat membantu Anda menentukan nilai sebenarnya.
Jual di Pasar Antik atau Pameran Barang Antik
Menghadiri pameran barang antik atau pasar antik lokal bisa menjadi cara yang efektif untuk menjual barang-barang antik Anda kepada para kolektor atau penggemar. Ini juga bisa menjadi kesempatan untuk menarik minat lebih banyak pembeli potensial.
Platform Online Khusus Barang Antik
Gunakan platform online yang khusus untuk menjual barang-barang antik. Situs seperti eBay, Etsy, Ruby Lane, atau situs lelang khusus antik bisa menjadi tempat yang baik untuk menjangkau pasar yang lebih luas.
Hubungi Pedagang atau Penjual Barang Antik
Menghubungi pedagang barang antik atau toko antik lokal bisa menjadi opsi lain. Mereka mungkin tertarik membeli barang-barang antik yang Anda miliki untuk kemudian mereka jual kembali di toko mereka.
Pemasaran dengan Presentasi yang Menarik
Ketika menjual barang antik, presentasi juga penting. Pastikan barang Anda diperlihatkan dengan baik melalui foto yang bagus, deskripsi yang jelas, dan jika perlu, cerita atau sejarah di balik barang tersebut.
Konsultasi dengan Ahli Antik
Jika Anda ragu tentang nilai atau cara terbaik untuk menjual barang antik Anda, berkonsultasilah dengan ahli antik. Mereka dapat memberikan saran tentang nilai pasar dan strategi penjualan terbaik.
Jangan Buru-buru dalam Penjualan
Ingatlah bahwa barang-barang antik mungkin memerlukan waktu untuk menemukan pembeli yang tepat. Jangan terburu-buru dalam menjualnya jika belum mendapatkan penawaran yang sesuai dengan harapan Anda.
Menjual barang antik bisa menjadi peluang yang menarik, tetapi dibutuhkan kesabaran, pengetahuan, dan strategi yang tepat. Selalu pastikan untuk melakukan riset, mengetahui nilai sebenarnya dari barang-barang antik Anda, dan menggunakan platform yang tepat untuk menjangkau pasar yang lebih luas.
9 Barang Antik Termahal di Dunia, Ada yang Tembus Rp6 T – Barang antik adalah benda atau artefak yang telah berumur puluhan, ratusan, atau bahkan ribuan tahun. Barang antik ini sering kali memiliki nilai estetika, sejarah, atau keunikan yang membuatnya diminati oleh para kolektor, museum, atau individu yang menyukai barang-barang kuno. Barang antik bisa mencakup berbagai hal, mulai dari perabotan, keramik, lukisan, perhiasan, hingga benda-benda rumah tangga dan arsitektural. Salah satu faktor utama dalam menentukan apakah suatu barang dianggap antik adalah usianya. Biasanya, barang yang berumur minimal 100 tahun atau lebih dianggap sebagai barang antik.
Barang antik tidak hanya dihargai karena usianya yang tua, tetapi juga karena nilai historis, artistik, dan keunikan yang melekat pada barang tersebut. Nilai suatu barang antik bisa sangat bervariasi tergantung pada permintaan pasar, keadaan kondisi, dan asal usul barang itu sendiri. Koleksi barang antik dapat menjadi sumber kebanggaan, warisan budaya, atau investasi untuk masa depan, tetapi memerlukan pemahaman yang baik tentang pasar dan perawatan yang tepat untuk memastikan nilainya tetap terjaga.
Beberapa contoh barang antik termahal yang telah terjual di lelang atau pasar antik adalah:

Lukisan “Salvator Mundi” karya Leonardo da Vinci
Lukisan ini terjual dengan harga lebih dari $450 juta, menjadikannya salah satu lukisan termahal di dunia.
Berbagai Porselen dan Keramik Kuno
Barang-barang porselen atau keramik kuno dari dinasti-dinasti China atau Eropa, seperti vas atau piring langka, telah terjual dengan harga puluhan hingga ratusan juta dolar.
Perhiasan Bersejarah dengan Batu Berharga Besar
Beberapa perhiasan bersejarah yang memiliki batu berharga besar, seperti berlian atau safir, telah terjual dengan harga yang sangat tinggi di pasar antik.
Mobil Klasik Langka
Mobil klasik yang langka dan memiliki sejarah tertentu, seperti Ferrari 250 GTO, telah terjual dengan harga puluhan juta dolar.
Harga yang fantastis untuk barang-barang antik ini sering kali terkait dengan keunikan, kondisi, nilai sejarah, atau keterkaitan dengan tokoh-tokoh bersejarah yang penting. Informasi harga tersebut bisa ditemukan melalui sumber-sumber berita terkemuka, rumah lelang terkemuka, atau situs-situs spesialis dalam bidang barang-barang antik.
Berikut 5 Barang Antik Paling Diburu Kolektor – Barang antik adalah benda atau artefak yang telah berumur puluhan, ratusan, atau bahkan ribuan tahun. Barang antik ini sering kali memiliki nilai estetika, sejarah, atau keunikan yang membuatnya diminati oleh para kolektor, museum, atau individu yang menyukai barang-barang kuno. Barang antik bisa mencakup berbagai hal, mulai dari perabotan, keramik, lukisan, perhiasan, hingga benda-benda rumah tangga dan arsitektural. Salah satu faktor utama dalam menentukan apakah suatu barang dianggap antik adalah usianya. Biasanya, barang yang berumur minimal 100 tahun atau lebih dianggap sebagai barang antik.
Barang antik tidak hanya dihargai karena usianya yang tua, tetapi juga karena nilai historis, artistik, dan keunikan yang melekat pada barang tersebut. Nilai suatu barang antik bisa sangat bervariasi tergantung pada permintaan pasar, keadaan kondisi, dan asal usul barang itu sendiri. Koleksi barang antik dapat menjadi sumber kebanggaan, warisan budaya, atau investasi untuk masa depan, tetapi memerlukan pemahaman yang baik tentang pasar dan perawatan yang tepat untuk memastikan nilainya tetap terjaga.
Barang-barang antik yang paling diburu oleh para kolektor sering kali memiliki nilai sejarah yang tinggi, keunikan, atau keterkaitan dengan peristiwa penting dalam sejarah. Berikut adalah beberapa barang antik yang sering menjadi incaran para kolektor:

Lukisan Klasik oleh Seniman Terkenal
Lukisan-lukisan karya seniman terkenal seperti Leonardo da Vinci, Vincent van Gogh, Claude Monet, atau Pablo Picasso selalu menjadi incaran para kolektor. Lukisan-lukisan ini sering kali memiliki nilai artistik dan sejarah yang sangat tinggi.
Perhiasan Bersejarah
Perhiasan yang memiliki sejarah yang unik atau terkait dengan tokoh-tokoh bersejarah sering menjadi incaran para kolektor. Batu-batu berharga besar, seperti berlian atau safir, yang terdapat dalam perhiasan bersejarah juga sering dicari.
Porselen atau Keramik Kuno
Barang-barang porselen atau keramik kuno, terutama dari dinasti-dinasti Cina atau Eropa yang langka dan memiliki desain yang unik, sering menjadi incaran kolektor. Potongan-potongan porselen klasik ini memiliki nilai seni dan sejarah yang tinggi.
Antikuitas Klasik atau Artefak Bersejarah
Antikuitas atau artefak bersejarah dari peradaban kuno seperti patung-patung klasik, benda-benda keagamaan, atau benda-benda kuno yang terkait dengan sejarah penting selalu dicari oleh para kolektor yang tertarik pada sejarah kuno.
Buku-buku Langka atau Naskah Kuno
Naskah-naskah kuno, buku-buku langka, atau dokumen-dokumen bersejarah yang memiliki nilai pengetahuan dan sejarah yang tinggi sering menjadi incaran bagi kolektor buku antik.
Barang-barang antik ini menjadi sangat dicari karena memiliki nilai sejarah, artistik, atau keunikan yang tinggi. Kolektor yang tertarik pada nilai sejarah atau ingin memiliki potongan-potongan bersejarah sering kali menjadi pemburu utama barang-barang antik ini.
5 Barang Antik Termahal Sepanjang Masa yang Super Berharga – Barang antik adalah benda atau artefak yang telah berumur puluhan, ratusan, atau bahkan ribuan tahun. Barang antik ini sering kali memiliki nilai estetika, sejarah, atau keunikan yang membuatnya diminati oleh para kolektor, museum, atau individu yang menyukai barang-barang kuno. Barang antik bisa mencakup berbagai hal, mulai dari perabotan, keramik, lukisan, perhiasan, hingga benda-benda rumah tangga dan arsitektural. Salah satu faktor utama dalam menentukan apakah suatu barang dianggap antik adalah usianya. Biasanya, barang yang berumur minimal 100 tahun atau lebih dianggap sebagai barang antik.
Barang antik tidak hanya dihargai karena usianya yang tua, tetapi juga karena nilai historis, artistik, dan keunikan yang melekat pada barang tersebut. Nilai suatu barang antik bisa sangat bervariasi tergantung pada permintaan pasar, keadaan kondisi, dan asal usul barang itu sendiri. Koleksi barang antik dapat menjadi sumber kebanggaan, warisan budaya, atau investasi untuk masa depan, tetapi memerlukan pemahaman yang baik tentang pasar dan perawatan yang tepat untuk memastikan nilainya tetap terjaga.
Barang-barang antik dengan nilai tertinggi di pasaran sering kali memiliki nilai sejarah, keunikan, atau keterkaitan dengan tokoh-tokoh bersejarah yang penting. Beberapa barang antik termahal sepanjang masa yang dikenal memiliki harga fantastis di pasar antik adalah:

Lukisan “Salvator Mundi” karya Leonardo da Vinci
Lukisan ini dianggap sebagai karya terakhir Leonardo da Vinci yang ditemukan pada 2017. Lukisan ini terjual dalam lelang seharga lebih dari $450 juta, menjadikannya salah satu lukisan termahal di dunia.
Vase Qing Dynasty
Vase Qing Dynasty dari Dinasti Qing China dikenal karena keindahannya dan sejarahnya yang kaya. Sebuah vase Qing Dynasty terjual dengan harga lebih dari $80 juta dalam lelang.
Porselen Ming Dynasty
Barang-barang porselen dari Dinasti Ming China juga dikenal dengan nilai tinggi di pasar antik. Beberapa potongan porselen Ming Dynasty telah terjual dengan harga lebih dari $20 juta.
Mobil Klasik
Beberapa mobil klasik yang langka dan memiliki sejarah tertentu bisa dianggap sebagai barang antik dan terjual dengan harga fantastis di lelang. Contohnya, mobil Ferrari 250 GTO terjual dengan harga lebih dari $38 juta.
Berlian dan Perhiasan Bersejarah
Perhiasan dengan berlian besar atau batu permata langka yang memiliki sejarah khusus, seperti Hope Diamond, atau perhiasan yang terkait dengan tokoh-tokoh bersejarah, sering kali terjual dengan harga yang sangat tinggi di pasar antik.
Daftar ini hanya beberapa contoh barang antik termahal di dunia. Nilai yang tinggi dari barang-barang ini sering kali terkait dengan sejarah dan keunikan yang luar biasa. Harganya bisa sangat bervariasi tergantung pada keadaan pasar, nilai sejarah, dan minat kolektor pada waktu tertentu.
Hobi Koleksi Barang Antik Hasilkan Pundi-pundi Rupiah – Barang antik adalah benda atau artefak yang telah berumur puluhan, ratusan, atau bahkan ribuan tahun. Barang antik ini sering kali memiliki nilai estetika, sejarah, atau keunikan yang membuatnya diminati oleh para kolektor, museum, atau individu yang menyukai barang-barang kuno. Barang antik bisa mencakup berbagai hal, mulai dari perabotan, keramik, lukisan, perhiasan, hingga benda-benda rumah tangga dan arsitektural. Salah satu faktor utama dalam menentukan apakah suatu barang dianggap antik adalah usianya. Biasanya, barang yang berumur minimal 100 tahun atau lebih dianggap sebagai barang antik.
Barang antik tidak hanya dihargai karena usianya yang tua, tetapi juga karena nilai historis, artistik, dan keunikan yang melekat pada barang tersebut. Nilai suatu barang antik bisa sangat bervariasi tergantung pada permintaan pasar, keadaan kondisi, dan asal usul barang itu sendiri. Koleksi barang antik dapat menjadi sumber kebanggaan, warisan budaya, atau investasi untuk masa depan, tetapi memerlukan pemahaman yang baik tentang pasar dan perawatan yang tepat untuk memastikan nilainya tetap terjaga.
Hobi mengoleksi barang antik bisa menjadi cara yang menarik untuk menghasilkan pundi-pundi rupiah, terutama jika dilakukan dengan pengetahuan yang baik dan strategi yang tepat. Berikut adalah beberapa cara hobi koleksi barang antik dapat menjadi sumber penghasilan:

Pengetahuan dan Penelitian yang Mendalam
Dengan memahami pasar barang antik dan memiliki pengetahuan yang luas tentang jenis barang yang dikoleksi, Anda dapat mengidentifikasi potensi barang yang memiliki nilai tinggi di pasar.
Penjualan Kembali dengan Harga Lebih Tinggi
Jika Anda membeli barang antik dengan harga yang kompetitif atau di bawah nilai pasar, Anda bisa menjualnya kembali dengan harga yang lebih tinggi ketika nilai pasar naik. Ini memerlukan pemahaman yang baik tentang tren pasar dan nilai barang antik tersebut.
Restorasi dan Perbaikan
Jika Anda memiliki keterampilan dalam restorasi atau perbaikan barang antik, Anda dapat membeli barang yang kondisinya kurang baik dengan harga murah, memperbaikinya, dan menjualnya kembali dengan harga yang lebih tinggi setelah direstorasi.
Mengikuti Lelang atau Pameran
Berpartisipasi dalam lelang atau pameran barang antik bisa menjadi cara untuk menjual koleksi Anda kepada kolektor yang berminat atau dealer yang memiliki pengetahuan tentang nilai barang antik.
Jual Online atau Melalui Platform Khusus
Menggunakan platform online yang khusus untuk barang-barang antik, situs jual-beli, atau media sosial dapat membantu Anda mencapai pasar yang lebih luas.
Kemitraan dengan Galeri atau Toko Antik
Bekerjasama dengan galeri seni atau toko antik bisa menjadi opsi untuk menampilkan dan menjual koleksi barang antik Anda kepada para kolektor atau penggemar barang antik.
Selalu penting untuk melakukan penelitian yang mendalam, memahami nilai, dan keaslian barang antik yang Anda beli serta mengetahui kondisi pasar saat ini. Dengan memahami pasar dan memiliki strategi yang tepat, hobi koleksi barang antik bisa menjadi sumber penghasilan yang menguntungkan.
Berikut 5 Cara Jual Barang Antik, Bisa Untung Besar! – Barang antik adalah benda atau artefak yang telah berumur puluhan, ratusan, atau bahkan ribuan tahun. Barang antik ini sering kali memiliki nilai estetika, sejarah, atau keunikan yang membuatnya diminati oleh para kolektor, museum, atau individu yang menyukai barang-barang kuno. Barang antik bisa mencakup berbagai hal, mulai dari perabotan, keramik, lukisan, perhiasan, hingga benda-benda rumah tangga dan arsitektural. Salah satu faktor utama dalam menentukan apakah suatu barang dianggap antik adalah usianya. Biasanya, barang yang berumur minimal 100 tahun atau lebih dianggap sebagai barang antik.
Barang antik tidak hanya dihargai karena usianya yang tua, tetapi juga karena nilai historis, artistik, dan keunikan yang melekat pada barang tersebut. Nilai suatu barang antik bisa sangat bervariasi tergantung pada permintaan pasar, keadaan kondisi, dan asal usul barang itu sendiri. Koleksi barang antik dapat menjadi sumber kebanggaan, warisan budaya, atau investasi untuk masa depan, tetapi memerlukan pemahaman yang baik tentang pasar dan perawatan yang tepat untuk memastikan nilainya tetap terjaga.
Berikut adalah lima cara untuk menjual barang-barang antik dengan potensi untuk mendapatkan keuntungan yang besar:

Melalui Lelang Antik
Mengikuti lelang barang antik bisa menjadi cara yang efektif untuk menjual barang antik dengan nilai yang tinggi. Lelang antik menyediakan platform di mana kolektor dan peminat barang antik berkumpul, dan sering kali mencapai harga yang fantastis. Anda dapat bekerja sama dengan rumah lelang yang terkenal atau platform lelang online yang memiliki pengunjung yang besar.
Galeri Seni atau Toko Antik
Menjual barang antik melalui galeri seni atau toko antik adalah cara lain yang umum. Melalui galeri seni atau toko antik, Anda dapat menampilkan barang-barang antik Anda kepada calon pembeli yang berminat dan memiliki pengetahuan tentang nilai barang antik.
Jual Online di Situs Spesialis
Platform online khusus untuk barang-barang antik, seperti situs lelang online, situs jual-beli barang antik, atau platform spesialis untuk koleksi tertentu bisa menjadi pilihan. Anda dapat memanfaatkan gambar berkualitas tinggi dan deskripsi yang detail untuk menarik pembeli.
Partisipasi di Pameran Antik
Mengikuti pameran antik adalah cara lain untuk menjual barang antik Anda. Pameran ini sering kali menjadi tempat bertemunya kolektor dan peminat barang antik dari berbagai belahan dunia.
Kerjasama dengan Ahli atau Pialang Antik
Bekerjasama dengan ahli atau pialang antik yang memiliki pengalaman dapat membantu Anda dalam menemukan pembeli yang tepat untuk barang antik Anda. Mereka bisa memberikan saran tentang strategi penjualan yang efektif.
Sebelum menjual barang antik, pastikan Anda telah melakukan penelitian untuk mengetahui nilai dan sejarah barang tersebut, serta menjamin keaslian dan kondisi barang. Semua ini dapat meningkatkan peluang Anda untuk mendapatkan keuntungan yang besar saat menjual barang antik.
Ini Daftar Barang Antik yang Nilai Jualnya Sangat Fantastis – Barang antik adalah benda atau artefak yang telah berumur puluhan, ratusan, atau bahkan ribuan tahun. Barang antik ini sering kali memiliki nilai estetika, sejarah, atau keunikan yang membuatnya diminati oleh para kolektor, museum, atau individu yang menyukai barang-barang kuno. Barang antik bisa mencakup berbagai hal, mulai dari perabotan, keramik, lukisan, perhiasan, hingga benda-benda rumah tangga dan arsitektural. Salah satu faktor utama dalam menentukan apakah suatu barang dianggap antik adalah usianya. Biasanya, barang yang berumur minimal 100 tahun atau lebih dianggap sebagai barang antik.
Barang antik tidak hanya dihargai karena usianya yang tua, tetapi juga karena nilai historis, artistik, dan keunikan yang melekat pada barang tersebut. Nilai suatu barang antik bisa sangat bervariasi tergantung pada permintaan pasar, keadaan kondisi, dan asal usul barang itu sendiri. Koleksi barang antik dapat menjadi sumber kebanggaan, warisan budaya, atau investasi untuk masa depan, tetapi memerlukan pemahaman yang baik tentang pasar dan perawatan yang tepat untuk memastikan nilainya tetap terjaga.
Barang-barang antik dengan nilai jual yang fantastis sering kali memiliki sejarah, keunikan, atau keterkaitan dengan peristiwa-peristiwa penting dalam sejarah. Beberapa contoh barang antik yang nilainya jualnya sangat fantastis adalah:

Lukisan Karya Maestro Terkenal
Lukisan karya seniman-seniman terkenal seperti Leonardo da Vinci, Vincent van Gogh, atau Pablo Picasso dapat memiliki nilai jual fantastis di pasar seni. Lukisan-lukisan ini sering kali dilelang dengan harga yang sangat tinggi.
Barang-barang Porselen atau Keramik Klasik
Barang-barang porselen atau keramik dari dinasti kuno China atau Eropa yang langka dan memiliki desain yang unik dapat memiliki nilai jual yang fantastis di pasar antik internasional.
Perhiasan Bersejarah atau Berlian Langka
Perhiasan kuno dengan batu berharga langka, seperti berlian besar yang terkait dengan sejarah atau kepemilikan tokoh-tokoh terkenal, sering kali memiliki nilai jual yang fantastis di pasar antik.
Artefak Bersejarah atau Koleksi Budaya Kuno
Barang-barang bersejarah dari peradaban kuno, seperti patung-patung klasik, artefak bersejarah, atau barang-barang kuno yang terkait dengan peristiwa penting dalam sejarah, dapat memiliki nilai jual yang sangat tinggi.
Mebel atau Perabotan Kuno Bersejarah
Perabotan kuno yang terkait dengan sejarah penting atau kepemilikan oleh tokoh-tokoh terkenal sering kali memiliki nilai jual yang fantastis di pasar antik.
Nilai jual fantastis untuk barang-barang antik ini biasanya terkait dengan keunikan, keberadaan dalam kondisi yang baik, atau latar belakang historis yang luar biasa. Namun, perlu diingat bahwa nilai jualnya dapat bervariasi dan sangat dipengaruhi oleh kondisi pasar, keaslian, dan minat kolektor pada waktu tertentu.
5 Toko Barang Antik Bandung, Saatnya Berburu Koleksi Langka! – Barang antik adalah benda atau artefak yang telah berumur puluhan, ratusan, atau bahkan ribuan tahun. Barang antik ini sering kali memiliki nilai estetika, sejarah, atau keunikan yang membuatnya diminati oleh para kolektor, museum, atau individu yang menyukai barang-barang kuno. Barang antik bisa mencakup berbagai hal, mulai dari perabotan, keramik, lukisan, perhiasan, hingga benda-benda rumah tangga dan arsitektural. Salah satu faktor utama dalam menentukan apakah suatu barang dianggap antik adalah usianya. Biasanya, barang yang berumur minimal 100 tahun atau lebih dianggap sebagai barang antik.
Barang antik tidak hanya dihargai karena usianya yang tua, tetapi juga karena nilai historis, artistik, dan keunikan yang melekat pada barang tersebut. Nilai suatu barang antik bisa sangat bervariasi tergantung pada permintaan pasar, keadaan kondisi, dan asal usul barang itu sendiri. Koleksi barang antik dapat menjadi sumber kebanggaan, warisan budaya, atau investasi untuk masa depan, tetapi memerlukan pemahaman yang baik tentang pasar dan perawatan yang tepat untuk memastikan nilainya tetap terjaga.
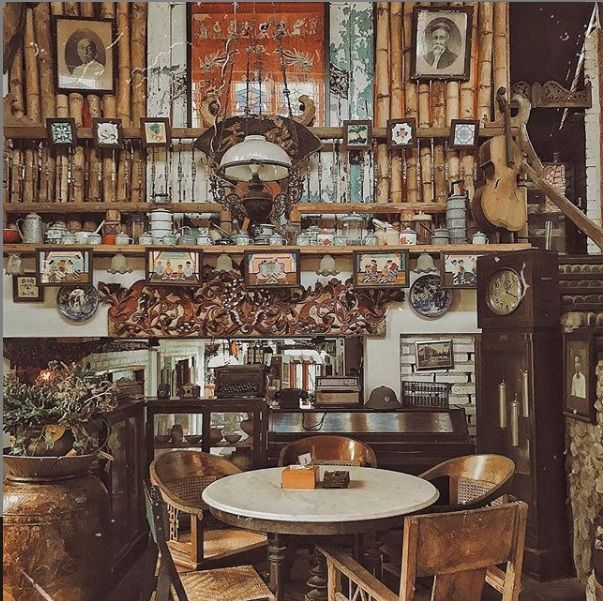
Namun, Bandung memiliki sejumlah tempat yang dapat menjadi tujuan bagi para kolektor barang antik. Beberapa daerah yang mungkin memiliki toko-toko barang antik di Bandung antara lain:

Jalan Braga
Jalan ini memiliki sejarah panjang di Bandung dan dikenal dengan keberadaan toko-toko antik, galeri seni, dan warung kopi yang menghadirkan nuansa masa lalu.
Dago Antik
Kawasan Dago memiliki beberapa toko antik yang menawarkan berbagai koleksi unik seperti perabotan klasik, kerajinan tangan kuno, dan barang-barang antik lainnya.
Cikutra
Di sepanjang Jalan Cikutra, terdapat beberapa toko yang menjual barang-barang antik dan koleksi klasik.
Jalan Riau
Jalan ini juga memiliki toko-toko yang menyediakan barang-barang antik dan koleksi unik lainnya.
Penting untuk melakukan penelitian lebih lanjut atau mencari informasi terkini secara online atau melalui sumber-sumber lokal di Bandung untuk mengetahui toko-toko barang antik yang saat ini tersedia di kota tersebut. Anda juga dapat menghubungi komunitas kolektor barang antik atau galeri seni yang mungkin memiliki informasi lebih lanjut tentang toko-toko tersebut.
5 Barang Antik Nilainya Sampai Triliunan Rupiah – Barang antik adalah benda atau artefak yang telah berumur puluhan, ratusan, atau bahkan ribuan tahun. Barang antik ini sering kali memiliki nilai estetika, sejarah, atau keunikan yang membuatnya diminati oleh para kolektor, museum, atau individu yang menyukai barang-barang kuno. Barang antik bisa mencakup berbagai hal, mulai dari perabotan, keramik, lukisan, perhiasan, hingga benda-benda rumah tangga dan arsitektural.
Barang antik tidak hanya dihargai karena usianya yang tua, tetapi juga karena nilai historis, artistik, dan keunikan yang melekat pada barang tersebut. Nilai suatu barang antik bisa sangat bervariasi tergantung pada permintaan pasar, keadaan kondisi, dan asal usul barang itu sendiri. Koleksi barang antik dapat menjadi sumber kebanggaan, warisan budaya, atau investasi untuk masa depan, tetapi memerlukan pemahaman yang baik tentang pasar dan perawatan yang tepat untuk memastikan nilainya tetap terjaga.
Berikut beberapa contoh barang antik dengan nilai tinggi:
Lukisan Klasik atau Karya Seni Tertentu
Lukisan-lukisan karya pelukis terkenal atau lukisan era klasik yang langka bisa memiliki nilai yang sangat tinggi. Sebuah karya seni klasik yang dilukis oleh seniman terkenal seperti Leonardo da Vinci, Vincent van Gogh, atau Pablo Picasso dapat mencapai harga jutaan hingga triliunan rupiah di pasar lelang seni internasional.
Perhiasan Bersejarah dan Berlian Langka
Perhiasan kuno dengan batu berharga langka, seperti berlian besar dengan sejarah yang terkait dengan tokoh-tokoh bersejarah, dapat memiliki nilai sangat tinggi di pasar antik dan lelang.
Keramik Kuno atau Porselen Langka
Barang-barang porselen atau keramik klasik dari dinasti-dinasti kuno China atau Jepang, atau barang-barang porselen Eropa yang langka bisa mencapai nilai yang tinggi di pasar antik.
Perabotan Antik Bersejarah
Perabotan kuno dari periode tertentu atau yang terkait dengan tokoh-tokoh sejarah terkenal, seperti mebel kerajaan atau mebel yang terkait dengan pribadi penting dalam sejarah, bisa memiliki nilai yang sangat tinggi.
Koleksi Barang Kuno yang Langka
Beberapa koleksi antik yang jarang dan langka, seperti koleksi koin kuno yang langka, perangko klasik, atau benda-benda bersejarah dari peradaban kuno, dapat memiliki nilai yang mencapai triliunan rupiah di pasar antik.
Nilai triliunan rupiah untuk barang-barang antik ini sangat jarang terjadi, dan nilai tersebut sering kali terkait dengan sejarah yang luar biasa, keunikan yang sangat langka, atau keterkaitan dengan tokoh-tokoh bersejarah yang penting.
Berikut 7 Barang antik yang dipercaya berhantu – Barang antik adalah benda atau artefak yang telah berumur puluhan, ratusan, atau bahkan ribuan tahun. Barang antik ini sering kali memiliki nilai estetika, sejarah, atau keunikan yang membuatnya diminati oleh para kolektor, museum, atau individu yang menyukai barang-barang kuno. Barang antik bisa mencakup berbagai hal, mulai dari perabotan, keramik, lukisan, perhiasan, hingga benda-benda rumah tangga dan arsitektural.
Barang antik tidak hanya dihargai karena usianya yang tua, tetapi juga karena nilai historis, artistik, dan keunikan yang melekat pada barang tersebut. Nilai suatu barang antik bisa sangat bervariasi tergantung pada permintaan pasar, keadaan kondisi, dan asal usul barang itu sendiri. Koleksi barang antik dapat menjadi sumber kebanggaan, warisan budaya, atau investasi untuk masa depan, tetapi memerlukan pemahaman yang baik tentang pasar dan perawatan yang tepat untuk memastikan nilainya tetap terjaga.
Boneka atau Patung: Beberapa boneka atau patung kuno dianggap memiliki kehadiran spiritual atau energi negatif yang dikaitkan dengan cerita-cerita misterius atau kejadian aneh.

Lukisan Tertentu
Lukisan kuno atau gambar-gambar tertentu sering dihubungkan dengan cerita mistis atau legenda yang menimbulkan kepercayaan akan energi negatif.
Perabotan Kuno
Terkadang, perabotan kuno seperti lemari, kursi, atau meja juga diyakini memiliki aspek supranatural yang menyertainya, terutama jika memiliki sejarah atau kisah yang gelap.
Keramik atau Barang Porselen
Barang-barang antik berbahan keramik atau porselen yang memiliki latar belakang yang tidak jelas atau berasal dari tempat-tempat dengan sejarah mistis dapat dipercaya memiliki energi negatif.
Benda-benda Budaya atau Ritual
Benda-benda yang digunakan dalam praktik-praktik spiritual, seperti alat persembahan atau barang-barang upacara, sering kali dikaitkan dengan energi mistis atau paranormal.
Alat Musik Kuno
Musik box, alat musik tua, atau gramofon klasik dapat dihubungkan dengan cerita-cerita tentang keberadaan spiritual yang misterius.
Buku Tua atau Naskah Kuno
Buku-buku kuno atau naskah-naskah yang memiliki reputasi sebagai benda bersejarah atau berkaitan dengan praktik spiritual kadang-kadang dianggap memiliki pengaruh atau energi yang aneh.
Perlu diingat bahwa keyakinan akan hal-hal yang berhubungan dengan dunia supranatural sangatlah subjektif dan tergantung pada budaya, tradisi, atau cerita-cerita lokal. Ini bukanlah fakta ilmiah atau kebenaran universal. Bagi sebagian orang, barang-barang antik ini mungkin hanya memiliki nilai sejarah dan artistik tanpa keterkaitan dengan keberadaan hantu atau energi negatif.
6 Tips Sukses Saat Berinvestasi Perabotan Antik – Barang antik adalah benda atau artefak yang telah berumur puluhan, ratusan, atau bahkan ribuan tahun. Barang antik ini sering kali memiliki nilai estetika, sejarah, atau keunikan yang membuatnya diminati oleh para kolektor, museum, atau individu yang menyukai barang-barang kuno. Barang antik bisa mencakup berbagai hal, mulai dari perabotan, keramik, lukisan, perhiasan, hingga benda-benda rumah tangga dan arsitektural.
Barang antik tidak hanya dihargai karena usianya yang tua, tetapi juga karena nilai historis, artistik, dan keunikan yang melekat pada barang tersebut. Nilai suatu barang antik bisa sangat bervariasi tergantung pada permintaan pasar, keadaan kondisi, dan asal usul barang itu sendiri. Koleksi barang antik dapat menjadi sumber kebanggaan, warisan budaya, atau investasi untuk masa depan, tetapi memerlukan pemahaman yang baik tentang pasar dan perawatan yang tepat untuk memastikan nilainya tetap terjaga.
Berinvestasi dalam perabotan antik bisa menjadi pilihan yang menarik tetapi memerlukan pengetahuan dan pemahaman yang baik tentang pasar serta barang antik itu sendiri. Berikut adalah enam tips untuk sukses saat berinvestasi dalam perabotan antik:

Pendidikan dan Pengetahuan yang Mendalam
Pelajari tentang jenis perabotan antik yang Anda minati. Buku, kursus, dan penelitian online dapat membantu Anda memahami karakteristik, gaya, dan nilai pasar dari perabotan antik tertentu.
Kondisi dan Otentikasi
Pastikan Anda memahami standar kondisi yang baik untuk perabotan antik. Periksa keaslian barang tersebut dan verifikasi otentisitasnya melalui sumber yang terpercaya, seperti penilai antik atau ahli yang terkait.
Diversifikasi Portofolio
Berinvestasi dalam berbagai jenis perabotan antik dapat membantu melindungi investasi Anda. Diversifikasi memungkinkan Anda untuk menyeimbangkan risiko dan peluang keuntungan.
Hubungan dengan Ahli
Jalin hubungan dengan ahli perabotan antik atau kolektor berpengalaman. Mereka dapat memberikan saran berharga tentang tren pasar, kondisi terkini, dan potensi investasi yang baik.
Pasar dan Nilai
Pahami pasar tempat Anda berniat untuk berinvestasi. Pelajari tren harga, permintaan, dan nilai tertinggi yang terkait dengan jenis perabotan antik yang Anda minati.
Lindungi Investasi
Pastikan perabotan antik Anda dilindungi dengan baik. Ini termasuk asuransi yang memadai, perawatan yang tepat, dan penyimpanan yang aman untuk mencegah kerusakan atau kehilangan nilai.
Ingatlah bahwa pasar perabotan antik bisa fluktuatif, dan nilai bisa berubah seiring waktu. Melakukan investasi dalam perabotan antik memerlukan kesabaran, pengetahuan, dan pemahaman yang baik tentang pasar. Sebaiknya Anda melakukan riset yang menyeluruh dan berkonsultasi dengan ahli sebelum membuat keputusan investasi besar dalam perabotan antik.
Bisa Kaya Mendadak, Barang Antik Ini Harga Miliaran di Indo – Barang antik adalah benda-benda yang telah ada sejak lama, sering kali berasal dari zaman kuno hingga zaman yang lebih baru, yang memiliki nilai historis, artistik, atau keunikan yang membuatnya menjadi objek koleksi yang diminati oleh para kolektor. Barang antik biasanya memiliki usia yang sudah cukup tua, sering kali berusia puluhan hingga ratusan tahun.
Barang antik memiliki daya tarik bagi banyak orang karena merupakan jendela ke masa lalu. Koleksi barang antik sering kali menjadi bagian dari kekayaan budaya dan sejarah suatu komunitas atau bangsa. Ketertarikan terhadap barang-barang ini juga dapat dijelaskan oleh nilai estetika, keingintahuan akan sejarah, atau nilai koleksi yang meningkat seiring dengan waktu. pafikebasen.org
Beberapa barang antik memiliki nilai yang sangat tinggi di pasar koleksi Indonesia dan dapat terjual dengan harga miliaran rupiah. Beberapa contoh barang antik yang bisa memiliki harga tinggi di Indonesia antara lain:

Keris-Keris Langka
Keris adalah senjata tradisional Indonesia yang memiliki nilai historis dan seni tinggi. Keris langka dari zaman kerajaan atau keris kuno dengan pamor tertentu bisa memiliki harga jutaan hingga miliaran rupiah.
Lukisan Klasik
Lukisan klasik dari pelukis ternama atau karya seni rupa Indonesia yang langka bisa memiliki nilai tinggi di pasar seni. Lukisan dari seniman seperti Raden Saleh atau Affandi bisa mencapai harga miliaran rupiah.
Perhiasan Bersejarah
Perhiasan antik dari zaman kerajaan atau masa lampau Indonesia yang terbuat dari emas, perak, atau batu permata langka bisa memiliki harga yang sangat tinggi di pasar koleksi.
Keramik dan Porselen Kuno
Vas, piring, atau patung dari keramik atau porselen kuno dari zaman Majapahit atau kerajaan-kerajaan lainnya memiliki nilai tinggi bagi para kolektor dan bisa terjual dengan harga yang fantastis.
Prangko Langka
Prangko atau perangko kuno yang langka dari masa kolonial atau masa lampau Indonesia dapat memiliki nilai koleksi yang tinggi di kalangan numismatis.
Perabotan Klasik
Perabotan klasik dari kayu atau logam dari zaman kolonial atau zaman kerajaan Indonesia bisa menjadi barang antik yang memiliki nilai tinggi di pasar koleksi.
Perlu dicatat bahwa harga barang antik sangat dipengaruhi oleh faktor keunikan, keadaan, provenans, dan permintaan pasar pada waktu tertentu. Investasi dalam barang-barang antik memerlukan pengetahuan mendalam tentang koleksi serta konsultasi dengan ahli dan kolektor yang berpengalaman untuk memastikan keaslian dan nilai dari barang antik tersebut.
Toko Barang Antik di Medan, Jual Radio Kuno Hingga Lukisan – Barang antik adalah benda-benda yang telah ada sejak lama, sering kali berasal dari zaman kuno hingga zaman yang lebih baru, yang memiliki nilai historis, artistik, atau keunikan yang membuatnya menjadi objek koleksi yang diminati oleh para kolektor. Barang antik biasanya memiliki usia yang sudah cukup tua, sering kali berusia puluhan hingga ratusan tahun.
Barang antik memiliki daya tarik bagi banyak orang karena merupakan jendela ke masa lalu. Koleksi barang antik sering kali menjadi bagian dari kekayaan budaya dan sejarah suatu komunitas atau bangsa. Ketertarikan terhadap barang-barang ini juga dapat dijelaskan oleh nilai estetika, keingintahuan akan sejarah, atau nilai koleksi yang meningkat seiring dengan waktu. Ketika mengoleksi barang antik, penting untuk memperhatikan keaslian, kondisi, dan nilai yang terkait dengan objek tersebut. Karena keunikan dan keterbatasan jumlah barang antik yang ada, minat terhadapnya sering kali meningkatkan nilai dan popularitasnya di pasar koleksi. https://pafikebasen.org/
Di Medan, terdapat beberapa tempat yang mungkin menjual barang-barang antik termasuk radio kuno dan lukisan-lukisan klasik. Berikut beberapa tempat yang mungkin dapat Anda kunjungi:

Pasar Johar Medan
Pasar ini dikenal memiliki sejumlah lapak yang menjual barang-barang antik termasuk barang-barang koleksi seperti radio kuno dan barang antik lainnya. Anda bisa menjelajahi area ini untuk mencari barang yang diinginkan.
Pasar Petisah
Pasar yang sudah terkenal sejak lama di Medan ini memiliki beragam lapak yang menjual barang-barang antik, mulai dari perabotan tua, perhiasan, hingga barang-barang koleksi lainnya.
Toko Antik Sei Sikambing
Toko ini juga terkenal menjual berbagai barang antik termasuk radio kuno, perabotan klasik, lukisan, dan barang-barang antik lainnya. Anda bisa mencari barang yang diinginkan di toko ini.
Toko Antik di Jalan Thamrin
Di sepanjang Jalan Thamrin, terdapat beberapa toko antik yang menjual beragam barang antik termasuk radio kuno, lukisan, dan koleksi lainnya.
Pastikan untuk melakukan pengecekan lebih lanjut atau konfirmasi terlebih dahulu melalui telepon atau situs web jika ada, karena ketersediaan barang dan barang apa yang tersedia di toko-toko antik dapat bervariasi dari waktu ke waktu.
Berikut Daftar 7 Barang Antik Paling Dicari Kolektor Indo – Barang antik adalah benda-benda yang telah ada sejak lama, sering kali berasal dari zaman kuno hingga zaman yang lebih baru, yang memiliki nilai historis, artistik, atau keunikan yang membuatnya menjadi objek koleksi yang diminati oleh para kolektor. Barang antik biasanya memiliki usia yang sudah cukup tua, sering kali berusia puluhan hingga ratusan tahun.
Barang antik memiliki daya tarik bagi banyak orang karena merupakan jendela ke masa lalu. Koleksi barang antik sering kali menjadi bagian dari kekayaan budaya dan sejarah suatu komunitas atau bangsa. Ketertarikan terhadap barang-barang ini juga dapat dijelaskan oleh nilai estetika, keingintahuan akan sejarah, atau nilai koleksi yang meningkat seiring dengan waktu.
Di Indonesia, kolektor barang antik mencari sejumlah barang khusus yang memiliki nilai historis, budaya, dan artistik yang tinggi. Berikut adalah daftar tujuh barang antik yang sering dicari oleh kolektor di Indonesia:

Keramik Kuno Indonesia
Keramik kuno dari berbagai daerah di Indonesia seperti Majapahit, Cirebon, atau keramik dari era Hindia Belanda menjadi barang antik yang dicari oleh kolektor di Indonesia.
Wayang Kulit dan Wayang Golek
Wayang kulit tradisional atau wayang golek dengan nilai sejarah dan seni tinggi seringkali menjadi objek yang dicari oleh kolektor seni rupa tradisional Indonesia.
Keris dan Senjata Kuno
Keris, senjata tradisional yang memiliki nilai simbolis dan artistik tinggi, serta senjata kuno lainnya seperti tombak atau golok, menjadi objek koleksi yang sangat diminati.
Uang Kuno dan Mata Uang
Koin kuno, uang logam, atau uang kertas dari zaman kolonial atau masa lampau Indonesia menjadi barang antik yang sering dicari oleh kolektor numismatis.
Prangko dan Dokumen Pos Lama
Prangko atau perangko lama dari zaman kolonial atau masa perjuangan kemerdekaan, serta dokumen-dokumen pos kuno, menjadi objek koleksi yang populer.
Piring dan Peralatan Makan Kuno
Piring-piring kuno, mangkuk, atau peralatan makan lainnya dari keramik atau porselen dengan desain tradisional atau zaman kolonial menjadi barang antik yang dicari.
Buku dan Dokumen Bersejarah
Buku-buku langka, manuskrip kuno, atau dokumen bersejarah lainnya seperti surat-surat dari zaman kolonial Indonesia menjadi barang antik yang populer bagi para kolektor.
Barang-barang antik ini memiliki nilai sejarah, budaya, dan keunikan yang tinggi, yang membuatnya menjadi objek yang diminati oleh para kolektor di Indonesia untuk memperkaya dan melestarikan warisan budaya bangsa.
Ini 9 Barang Antik Termahal di Dunia, Kolektor Wajib Tahu! – Barang antik adalah benda-benda yang telah ada sejak lama, sering kali berasal dari zaman kuno hingga zaman yang lebih baru, yang memiliki nilai historis, artistik, atau keunikan yang membuatnya menjadi objek koleksi yang diminati oleh para kolektor. Barang antik biasanya memiliki usia yang sudah cukup tua, sering kali berusia puluhan hingga ratusan tahun.
Barang antik memiliki daya tarik bagi banyak orang karena merupakan jendela ke masa lalu. Koleksi barang antik sering kali menjadi bagian dari kekayaan budaya dan sejarah suatu komunitas atau bangsa. Ketertarikan terhadap barang-barang ini juga dapat dijelaskan oleh nilai estetika, keingintahuan akan sejarah, atau nilai koleksi yang meningkat seiring dengan waktu. www.century2.org
Terdapat banyak barang antik yang telah terjual dengan harga fantastis di pasar koleksi. Berikut adalah sembilan contoh barang antik termahal di dunia yang telah tercatat dalam transaksi penjualan yang mencengangkan:

Keramik Song Dynasty
Sebuah mangkuk keramik dari Dinasti Song Tiongkok kuno terjual dengan harga sekitar 37,7 juta dolar AS pada lelang pada tahun 2017. Mangkuk ini menjadi salah satu keramik paling mahal yang pernah terjual.
Lukisan “Salvator Mundi” karya Leonardo da Vinci
Lukisan ini merupakan salah satu karya terkenal Leonardo da Vinci dan terjual dengan harga mencapai 450,3 juta dolar AS pada lelang Christie’s pada tahun 2017, menjadikannya lukisan termahal yang pernah terjual.
Koin Flowing Hair Dollar
Sebuah koin Flowing Hair Dollar yang diproduksi pada tahun 1794 di Amerika Serikat terjual seharga 10 juta dolar AS pada lelang pada tahun 2013. Koin ini adalah salah satu koin paling langka dan mahal di dunia.
Meja Sekretaris dari era Ratu Anne
Meja sekretaris yang terbuat dari kayu mahoni pada era Ratu Anne pada abad ke-18 terjual seharga 8,6 juta dolar AS pada lelang pada tahun 2008.
Koleksi Perhiasan Marie Antoinette
Koleksi perhiasan yang pernah dimiliki oleh Ratu Perancis Marie Antoinette terjual dengan harga sekitar 44 juta dolar AS pada lelang pada tahun 2018.
Harga barang-barang antik tersebut dapat sangat bervariasi tergantung pada keunikan, kondisi, sejarah, dan permintaan pasar pada saat penjualan. Barang-barang ini menjadi bukti nyata tentang minat yang tinggi dalam koleksi barang-barang antik yang berharga.
Ini 7 Rekomendasi Barang Antik untuk Koleksi Anda – Barang antik adalah benda-benda yang telah ada sejak lama, sering kali berasal dari zaman kuno hingga zaman yang lebih baru, yang memiliki nilai historis, artistik, atau keunikan yang membuatnya menjadi objek koleksi yang diminati oleh para kolektor. Barang antik biasanya memiliki usia yang sudah cukup tua, sering kali berusia puluhan hingga ratusan tahun.
Barang antik memiliki daya tarik bagi banyak orang karena merupakan jendela ke masa lalu. Koleksi barang antik sering kali menjadi bagian dari kekayaan budaya dan sejarah suatu komunitas atau bangsa. Ketertarikan terhadap barang-barang ini juga dapat dijelaskan oleh nilai estetika, keingintahuan akan sejarah, atau nilai koleksi yang meningkat seiring dengan waktu. https://www.century2.org/
Tentu, berikut adalah tujuh rekomendasi barang antik yang dapat menjadi koleksi menarik:

Koin Kuno atau Uang Logam
Koin atau uang logam dari berbagai zaman atau negara yang langka bisa menjadi koleksi yang menarik bagi para numismatis atau kolektor uang kuno.
Keramik atau Porselen Bersejarah
Vas, piring, atau patung dari keramik atau porselen dengan desain klasik atau dari manufaktur terkenal pada masa lalu sering menjadi objek koleksi yang bernilai.
Lukisan atau Karya Seni Klasik
Lukisan klasik dari pelukis terkenal atau karya seni lainnya seperti patung atau ukiran kayu dari periode sejarah tertentu memiliki nilai koleksi yang tinggi.
Perhiasan Antik
Perhiasan dari logam mulia atau batu permata langka dari zaman kuno yang memiliki nilai artistik dan sejarah dapat menjadi koleksi yang istimewa.
Buku atau Manuskrip Lama
Buku kuno, manuskrip langka, atau buku dengan edisi terbatas, terutama yang memiliki tanda tangan penulis terkenal, juga menjadi objek koleksi yang diminati.
Perabotan Antik
Perabotan kuno seperti meja, kursi, lemari, atau jam dinding dengan desain klasik atau gaya tertentu bisa menjadi koleksi yang menarik bagi para kolektor perabotan antik.
Barang-barang Logam Berharga
Barang dari logam berharga seperti arloji, vas, atau barang perak, emas, atau tembaga kuno dengan nilai seni yang tinggi juga menjadi objek koleksi yang dicari.
Saat memilih barang-barang antik untuk dikoleksi, penting untuk memperhatikan kondisi, keaslian, dan nilai dari barang tersebut. Melakukan riset, berbicara dengan ahli, atau bergabung dalam komunitas kolektor dapat membantu Anda memilih barang antik yang sesuai dengan minat dan keinginan koleksi Anda.
Berikut 8 Barang Antik Pemanis Sudut Hunian – Barang antik adalah benda-benda yang telah ada sejak lama, sering kali berasal dari zaman kuno hingga zaman yang lebih baru, yang memiliki nilai historis, artistik, atau keunikan yang membuatnya menjadi objek koleksi yang diminati oleh para kolektor. Barang antik biasanya memiliki usia yang sudah cukup tua, sering kali berusia puluhan hingga ratusan tahun.
Barang antik memiliki daya tarik bagi banyak orang karena merupakan jendela ke masa lalu. Koleksi barang antik sering kali menjadi bagian dari kekayaan budaya dan sejarah suatu komunitas atau bangsa. Ketertarikan terhadap barang-barang ini juga dapat dijelaskan oleh nilai estetika, keingintahuan akan sejarah, atau nilai koleksi yang meningkat seiring dengan waktu. www.creeksidelandsinn.com
Terdapat banyak barang antik yang bisa menjadi pemanis sudut hunian dan memberikan sentuhan istimewa pada dekorasi rumah. Berikut adalah delapan contoh barang antik yang dapat menjadi pemanis sudut hunian:

Lampu Gantung Antik
Lampu gantung klasik dari periode tertentu bisa menjadi sorotan di ruangan dan memberikan nuansa vintage yang menarik.
Jam Dinding Klasik
Jam dinding klasik dari kayu, tembaga, atau logam yang telah ada sejak lama bisa menjadi barang antik yang menarik dan berfungsi dengan baik sebagai hiasan.
Keramik atau Porselen Bersejarah
Vas, piring, atau patung klasik dari keramik atau porselen dengan desain klasik bisa menjadi titik fokus yang menawan.
Kursi atau Meja Antik
Kursi kayu tua, sofa retro, atau meja makan dengan desain klasik yang terawat baik bisa memberikan sentuhan elegan pada ruangan.
Kotak Musisi atau Gramofon
Barang antik seperti kotak musik tua atau gramofon bisa menjadi barang koleksi yang menarik dan memberikan nuansa nostalgia.
Peta atau Peta Rencana Lama
Peta geografis atau peta rencana lama yang di-frame dengan baik dapat memberikan dekorasi dinding yang menarik dan edukatif.
Kaca Cermin Kuno
Cermin dengan bingkai klasik atau model kuno dapat memberikan sentuhan artistik dan elegan pada ruang yang ditempati.
Mesin Tik atau Mesin Ketik Lama
Mesin ketik klasik atau mesin tik lama yang masih berfungsi bisa menjadi hiasan menarik di sudut ruangan.
Memilih barang antik untuk dekorasi rumah membutuhkan perhatian terhadap keseluruhan tema dan gaya dekorasi ruangan. Pastikan barang antik yang Anda pilih dapat berintegrasi dengan baik dalam ruangannya dan menjadi pemanis yang menyatu dengan dekorasi keseluruhan.
Dulu Mahal, Kini 6 Benda Antik Ini Perlu Dibuang – Barang antik adalah benda-benda yang telah ada sejak lama, sering kali berasal dari zaman kuno hingga zaman yang lebih baru, yang memiliki nilai historis, artistik, atau keunikan yang membuatnya menjadi objek koleksi yang diminati oleh para kolektor. Barang antik biasanya memiliki usia yang sudah cukup tua, sering kali berusia puluhan hingga ratusan tahun.
Barang antik memiliki daya tarik bagi banyak orang karena merupakan jendela ke masa lalu. Koleksi barang antik sering kali menjadi bagian dari kekayaan budaya dan sejarah suatu komunitas atau bangsa. Ketertarikan terhadap barang-barang ini juga dapat dijelaskan oleh nilai estetika, keingintahuan akan sejarah, atau nilai koleksi yang meningkat seiring dengan waktu. https://www.creeksidelandsinn.com/
Terkadang, barang-barang antik yang dahulu dianggap bernilai tinggi bisa kehilangan daya tariknya atau nilai koleksinya seiring berjalannya waktu. Berikut adalah enam contoh barang antik yang mungkin saat ini perlu dipertimbangkan untuk dibuang:

Piring, Gelas, atau Keramik Rusak Berat
Barang-barang keramik atau porselen yang retak, pecah, atau rusak berat umumnya kehilangan nilai koleksinya.
Barang-barang Elektronik Kuno yang Tidak Berfungsi
Elektronik kuno seperti radio tua, mesin tik, atau perekam kaset yang tidak berfungsi atau sulit untuk diperbaiki mungkin tidak memiliki nilai koleksi yang tinggi lagi.
Majalah atau Koran Lama yang Tidak Terawat
Majalah atau koran kuno yang terlalu usang, kotor, atau rusak mungkin tidak lagi memiliki nilai tinggi bagi kolektor.
Perhiasan yang Tidak Terawat
Perhiasan kuno yang rusak, hilang bagian, atau terlalu aus mungkin kehilangan nilai koleksinya.
Buku-buku yang Terlalu Rusak atau Tidak Langka
Buku kuno yang terlalu rusak, tercemar, atau buku yang bukan edisi langka mungkin kurang diminati oleh kolektor.
Karya Seni yang Diragukan Keasliannya
Karya seni atau barang seni rupa yang terduga palsu atau memiliki keraguan tentang keaslian atau provenansinya bisa kehilangan nilai.
Sebelum membuang barang-barang antik tersebut, penting untuk memeriksa apakah barang tersebut benar-benar tidak berharga lagi atau masih bisa memiliki nilai sentimental bagi Anda atau mungkin bisa diperbaiki untuk mendapatkan nilai yang lebih baik. Jika Anda ragu, konsultasikan dengan ahli barang antik atau kolektor lainnya untuk saran dan penilaian lebih lanjut sebelum mengambil keputusan untuk membuangnya.
Berikut 7 Tips Investasi Barang Antik Untuk Anda Yang Gemar – Barang antik adalah benda-benda yang telah ada sejak lama, sering kali berasal dari zaman kuno hingga zaman yang lebih baru, yang memiliki nilai historis, artistik, atau keunikan yang membuatnya menjadi objek koleksi yang diminati oleh para kolektor. Barang antik biasanya memiliki usia yang sudah cukup tua, sering kali berusia puluhan hingga ratusan tahun.
Barang antik memiliki daya tarik bagi banyak orang karena merupakan jendela ke masa lalu. Koleksi barang antik sering kali menjadi bagian dari kekayaan budaya dan sejarah suatu komunitas atau bangsa. Ketertarikan terhadap barang-barang ini juga dapat dijelaskan oleh nilai estetika, keingintahuan akan sejarah, atau nilai koleksi yang meningkat seiring dengan waktu. hari88
Tentu, berikut adalah tujuh tips untuk investasi dalam barang-barang antik bagi para pecinta koleksi:

Pengetahuan yang Mendalam
Pelajari dan tingkatkan pengetahuan Anda tentang jenis barang antik yang ingin Anda koleksi. Mengetahui sejarah, asal-usul, dan karakteristik khusus dari setiap barang antik akan membantu Anda dalam membuat keputusan yang tepat.
Kondisi dan Keaslian
Pastikan Anda memahami kondisi barang antik yang ingin Anda beli. Keaslian dan keadaan barang menjadi faktor penting dalam menentukan nilai barang antik tersebut di pasar.
Jaringan dan Sumber yang Terpercaya
Bangun jaringan dengan kolektor lainnya, ahli, dan pedagang yang terpercaya. Berkomunikasi dengan mereka untuk mendapatkan informasi terkini dan saran-saran berharga mengenai investasi dalam barang-barang antik.
Diversifikasi Koleksi
Diversifikasi koleksi Anda dengan memilih berbagai jenis barang antik. Tidak hanya membatasi diri pada satu jenis barang, tetapi juga mempertimbangkan variasi koleksi untuk mengurangi risiko.
Perhatikan Perubahan Pasar
Monitor dan perhatikan tren pasar serta perkembangan harga di pasar barang antik. Pengetahuan mengenai pasar akan membantu Anda dalam mengambil keputusan investasi yang cerdas.
Lindungi Koleksi
Pastikan untuk menyimpan dan merawat koleksi barang antik Anda dengan baik. Penyimpanan yang tepat dan perawatan yang cermat akan menjaga nilai dari barang-barang antik tersebut.
Bersabar dan Mengikuti Insting
Investasi dalam barang-barang antik membutuhkan kesabaran. Tidak semua barang antik akan memberikan keuntungan seketika, namun jika Anda memiliki pengetahuan dan insting yang baik, hal ini dapat membawa keuntungan di masa depan.
Ingatlah bahwa pasar barang antik dapat fluktuatif, dan nilai barang-barang antik dapat berubah seiring waktu. Memiliki pemahaman yang baik tentang barang-barang antik yang Anda pilih untuk dikoleksi, serta melakukan riset yang mendalam sebelum berinvestasi, sangatlah penting.
8 Barang Antik Paling Dicari, Harganya Capai Ratusan Juta! – Barang antik adalah benda-benda yang telah ada sejak lama, sering kali berasal dari zaman kuno hingga zaman yang lebih baru, yang memiliki nilai historis, artistik, atau keunikan yang membuatnya menjadi objek koleksi yang diminati oleh para kolektor. Barang antik biasanya memiliki usia yang sudah cukup tua, sering kali berusia puluhan hingga ratusan tahun.
Barang antik memiliki daya tarik bagi banyak orang karena merupakan jendela ke masa lalu. Koleksi barang antik sering kali menjadi bagian dari kekayaan budaya dan sejarah suatu komunitas atau bangsa. Ketertarikan terhadap barang-barang ini juga dapat dijelaskan oleh nilai estetika, keingintahuan akan sejarah, atau nilai koleksi yang meningkat seiring dengan waktu. Ketika mengoleksi barang antik, penting untuk memperhatikan keaslian, kondisi, dan nilai yang terkait dengan objek tersebut. Karena keunikan dan keterbatasan jumlah barang antik yang ada, minat terhadapnya sering kali meningkatkan nilai dan popularitasnya di pasar koleksi.
Sejumlah barang antik memang memiliki nilai tinggi di pasar kolektor dan dapat mencapai harga yang sangat tinggi, bahkan mencapai ratusan juta. Berikut ini adalah beberapa barang antik yang sering dicari dan memiliki harga yang tinggi di pasar koleksi:
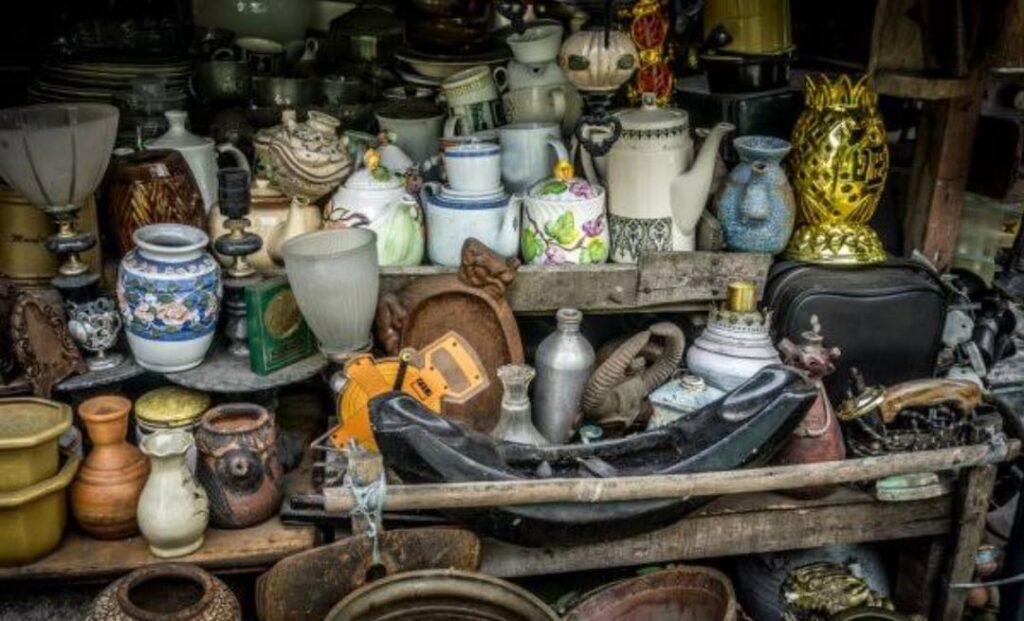
Karya Seni Lukisan Klasik
Lukisan-lukisan klasik karya pelukis terkenal dari zaman dahulu seringkali mencapai harga fantastis di pasar seni. Karya seni dari seniman terkenal seperti Rembrandt, Leonardo da Vinci, atau Vincent van Gogh dapat memperoleh harga yang sangat tinggi. https://hari88.net/
Perhiasan Berharga
Perhiasan antik, terutama perhiasan dengan berlian besar atau batu permata langka dari periode sejarah tertentu, sering kali memiliki nilai tinggi di pasar antik.
Karya Seni Klasik
Patung dan Ukiran Kayu: Patung atau ukiran kayu klasik dari periode tertentu, khususnya karya seni dari pengrajin terkenal, juga memiliki nilai tinggi di pasar koleksi.
Uang Kuno dan Mata Uang Langka
Koin kuno, uang kertas langka, atau mata uang dari masa lalu yang langka seringkali memiliki nilai koleksi yang tinggi, terutama jika kondisinya masih bagus.
Perabotan Antik
Perabotan kuno dari berbagai periode seperti meja, kursi, lemari, atau jam dinding yang dibuat dengan kualitas tinggi dan memiliki desain klasik juga menjadi incaran kolektor.
Keramik dan Porselen Kuno
Keramik atau porselen kuno dengan desain unik, motif yang langka, atau karya dari manufaktur terkenal dari masa lalu dapat memiliki nilai yang signifikan di pasar antik.
Barang-barang Logam Berharga
Barang-barang dari logam berharga seperti perhiasan antik, vas, arloji, atau barang tembaga, perak, atau emas kuno dengan nilai sejarah dan artistik yang tinggi juga menjadi objek koleksi yang mahal.
Buku-buku Langka
Buku-buku yang langka, khususnya edisi terbatas, buku kuno, manuskrip tua, atau buku dengan tanda tangan penulis terkenal dapat memiliki nilai koleksi yang tinggi.
Harga dari barang-barang antik ini sangat bervariasi dan tergantung pada keunikan, kondisi, usia, dan permintaan pasar saat itu. Koleksi barang-barang antik ini sering menjadi investasi yang berharga bagi para kolektor dengan kemungkinan nilai yang terus meningkat seiring waktu.
Berikut 5 Barang Antik Paling Diburu Kolektor – Barang antik adalah benda-benda yang telah ada sejak lama, sering kali berasal dari zaman kuno hingga zaman yang lebih baru, yang memiliki nilai historis, artistik, atau keunikan yang membuatnya menjadi objek koleksi yang diminati oleh para kolektor. Barang antik biasanya memiliki usia yang sudah cukup tua, sering kali berusia puluhan hingga ratusan tahun.
Barang antik memiliki daya tarik bagi banyak orang karena merupakan jendela ke masa lalu. Koleksi barang antik sering kali menjadi bagian dari kekayaan budaya dan sejarah suatu komunitas atau bangsa. Ketertarikan terhadap barang-barang ini juga dapat dijelaskan oleh nilai estetika, keingintahuan akan sejarah, atau nilai koleksi yang meningkat seiring dengan waktu. Ketika mengoleksi barang antik, penting untuk memperhatikan keaslian, kondisi, dan nilai yang terkait dengan objek tersebut. Karena keunikan dan keterbatasan jumlah barang antik yang ada, minat terhadapnya sering kali meningkatkan nilai dan popularitasnya di pasar koleksi.
Barang-barang antik seringkali menjadi incaran kolektor karena memiliki nilai historis, estetika, dan keunikan yang tinggi. Berikut adalah lima barang antik yang sering diburu oleh para kolektor:

Keramik dan Porselen
Barang-barang keramik atau porselen kuno dari berbagai zaman dan budaya sering menjadi objek koleksi yang dicari. Contohnya adalah piring, mangkuk, vas, atau patung-patung klasik yang memiliki nilai seni dan sejarah tinggi. hari88
Perabotan Antik
Perabotan kuno seperti meja, kursi, lemari, atau jam dinding yang memiliki desain klasik dan terbuat dari bahan-bahan berkualitas tinggi menjadi daya tarik bagi kolektor perabotan antik.
Uang Kuno dan Mata Uang
Koin kuno, uang kertas klasik, atau mata uang lama dari berbagai negara sering menjadi koleksi yang diminati oleh numismatis atau kolektor uang kuno.
Lukisan dan Karya Seni Klasik
Lukisan-lukisan klasik, ukiran kayu, patung, atau karya seni lainnya dari pelukis atau pengrajin terkenal di masa lalu juga termasuk dalam daftar barang antik yang sangat dicari oleh kolektor.
Barang-barang Logam Berharga
Benda-benda dari logam berharga seperti perhiasan antik, barang tembaga, perak, atau emas kuno dengan nilai sejarah, artistik, atau nilai koleksi tinggi menjadi incaran kolektor.
Tentu saja, nilai dan ketertarikan dalam mengumpulkan barang-barang antik sangatlah subjektif. Beberapa barang antik lainnya yang bisa menjadi objek koleksi meliputi perangko kuno, buku-buku langka, kamera tua, mainan antik, dan masih banyak lagi.
Do you know what are Healthcare Chatbots? Top 20 bot examples
For many people, it might be common sense not to feed ChatGPT PHI, source code, or proprietary information; however, some people might not fully understand the risks attached to it. As users of a growing number of AI technologies provided by private, for-profit companies, we should be extremely careful about what information we share with such tools. Undoubtedly, medical chatbots will become more accurate, but that alone won’t be enough to ensure their successful acceptance in the healthcare industry. As the healthcare industry is a mix of empathy and treatments, a similar balance will have to be created for chatbots to become more successful and accepted in the future.
- Using an AI chatbot can make the entire experience more personal and give them the impression they are speaking with a human.
- Leave us your details and explore the full potential of our future collaboration.
- Do you need to admit patients faster, automate appointment management, or provide additional services?
- Understanding these factors is crucial for the successful integration of chatbots in healthcare settings.
- However, these bots can at least help patients understand what kind of treatment to request and what might be the issue, which is already a good start.
Train your chatbot to be conversational and collect feedback in a casual and stress-free way. Healthcare chatbots are intelligent assistants used by medical centers and medical professionals to help patients get assistance faster. They can help with FAQs, appointment booking, reminders, and other repetitive questions or queries that often overload medical offices. However, https://chat.openai.com/ some of these were sketches of the interface rather than the final user interface, and most of the screenshots had insufficient description as to what the capabilities were. Although the technical descriptions of chatbots might constitute separate papers in their own right, these descriptions were outside the scope for our focus on evidence in public health.
Improved user engagement
One of the most critical considerations in implementing AI chatbots like ChatGPT is ensuring data security and privacy. This is even more important in highly regulated industries, such as health care delivery, pharmaceutical delivery, banking, and insurance, where AI tools collect client information. The lack of a robust AI security and privacy framework can result in data breaches, reputational damage, reduced consumer trust, compliance and regulatory violations, as well as heavy fines and penalties. ChatGPT, like any other technology used in the health care industry, must be used in compliance with HIPAA regulations.
With an AI chatbot, you can set up messages to be sent to patients with a personalized reminder. They can interact with the bot if they have more questions like their dosage, if they need a follow-up appointment, or if they have been experiencing any side effects that should be addressed. Although the use of NLP is a new territory in the health domain [47], it is a well-studied area in computer science and HCI.
Monitoring and Maintenance
Sensely is a tool that enables you to create and customize your own conversational AI solutions for health and wellness. I used Sensely’s chatbot to develop a virtual assistant for my fitness app, and I was impressed by how fast and easy it was. Hyro.ai also has a low cost of ownership, as it does not require any coding or complex integrations.
It uses natural language processing and artificial intelligence to deliver evidence-based interventions based on cognitive behavioral therapy. Smartbot360 is a HIPAA-compliant chatbot platform that provides secure communication between patients and providers. I used Kommunicate to automate my customer service for my healthcare business with the help of AI chatbots. Buoy Health uses natural language processing and artificial intelligence to thoroughly assess your symptoms, providing valuable insights into what’s going on. It also offers tailored recommendations, guiding you to appropriate healthcare resources like doctors, clinics, or telemedicine. As a healthcare provider, I was looking for a chatbot solution that could improve the quality and efficiency of my service.

In the light of the huge growth in the deployment of chatbots to support public health provision, there is pressing need for research to help guide their strategic development and application [13]. Reviewing current evidence, we identified some of the gaps in current knowledge and possible next steps for the development and use of chatbots for public health provision. So, healthcare providers can use a chatbot dedicated to answering their patient’s most commonly asked questions. Questions about insurance, like covers, claims, documents, symptoms, business hours, and quick fixes, can be communicated to patients through the chatbot.
GPT-4 surpasses ChatGPT in its advanced understanding and reasoning abilities and includes the ability to interact with images and longer text [20]. At present, GPT-4 is only accessible to those who have access to ChatGPT Plus, a premium service from OpenAI for which users have to pay US $20 a month. A healthcare chatbot can accomplish all of this and more by utilizing artificial intelligence and machine learning.
A chatbot can monitor available slots and manage patient meetings with doctors and nurses with a click. As for healthcare chatbot examples, Kyruus assists users in scheduling appointments with medical professionals. While AI chatbots offer many benefits, it is critical to understand their limitations.
Collects data for future reference
The gathering of patient information is one of the main applications of healthcare chatbots. By using healthcare chatbots, simple inquiries like the patient’s name, address, phone number, symptoms, current doctor, and insurance information can be utilized to gather information. Of course, no algorithm can compare to the experience of a doctor that’s earned in the field or the level of care a trained nurse can provide. However, chatbot solutions for the healthcare industry can effectively complement the work of medical professionals, saving time and adding value where it really counts. While AI chatbots can provide general recommendations, developing personalized treatment plans based on a patient’s unique circumstances, medical history, and preferences often requires the judgment and expertise of human healthcare providers.
I recommend Ada to anyone looking for a smart and effective chatbot for healthcare. Such fast processing of requests also adds to overall patient satisfaction and saves both doctors’ and patients’ time. Healthcare customer service chatbots can increase corporate Chat PG productivity without adding any additional costs or staff. This helps users to save time and hassle of visiting the clinic/doctor as by feeding in little information, one can easily get a nearly-accurate diagnosis with the help of these chatbots.
Personalized care
Infobip can help you jump start your conversational patient journeys using AI technology tools. Get an inside look at how to digitalize and streamline your processes while creating ethical and safe conversational journeys on any channel for your patients. Perfecting the use cases mentioned above would provide patients with comfortable, secure, and reliable conversations with their healthcare providers.
Use an AI chatbot to send automated messages, videos, images, and advice to patients in preparation for their appointment. The chatbot can easily converse with patients and answer any important questions they have at any time of day. The chatbot can also help remind patients of certain criteria to follow such as when to start fasting or how much water to drink before their appointment. So, how do healthcare centers and pharmacies incorporate AI chatbots without jeopardizing patient information and care?
While a website can provide information, it may not be able to address all patient queries. That’s where chatbots come in – they offer a more intuitive way for patients to get their questions answered and add a personal touch. In the event of a medical emergency, chatbots can instantly provide doctors with patient information such as medical history, allergies, past records, check-ups, and other important details.
USE CASES OF MEDICAL AI CHATBOTS (EXAMPLES INCLUDED)
The goals you set now will define the very essence of your new product, as well as the technology it will rely on. The process of filing insurance inquiries and claims is standardized and takes a lot of time to complete. You can foun additiona information about ai customer service and artificial intelligence and NLP. The solution provides information about insurance coverage, benefits, and claims information, allowing users to track and handle their health insurance-related needs conveniently.
Since its launch on November 30, 2022, ChatGPT, a free AI chatbot created by OpenAI [18], has gained over a million active users [19]. It is based on the GPT-3.5 foundation model, a powerful deep learning algorithm developed by OpenAI. It has been designed to simulate human conversation and provide human-like responses through text box services and voice commands [18].
As AI technologies become increasingly sophisticated, the potential for inadvertent disclosure of sensitive information may increase. For instance, health professionals may inadvertently reveal PHI if the original data were not adequately deidentified. How many times have you unintentionally copied and pasted your personal information such as login ID and password into Google search or the address bar? An acceptable use policy should stipulate a set of rules that a user must agree to for access to an AI tool. The policy should prevent a user from entering sensitive business or patient information into these AI tools.
As AI chatbots continue to evolve and improve, they are expected to play an even more significant role in healthcare, further streamlining processes and optimizing resource allocation. Healthcare insurance claims are complicated, stressful, and not something patients want to deal with, especially if they are in the middle of a health crisis. Using an AI chatbot for health insurance claims can help alleviate the stress of submitting a claim and improve the overall satisfaction of patients with your clinic. Answer questions about patient coverage and train the AI chatbot to navigate personal insurance plans to help patients understand what medical services are available to them. More broadly, in a rapidly developing technological field in which there is substantial investment from industry actors, there is a need for better reporting frameworks detailing the technologies and methods used for chatbot development. Finally, there is a need to understand and anticipate the ways in which these technologies might go wrong and ensure that adequate safeguarding frameworks are in place to protect and give voice to the users of these technologies.
A chatbot like that can be part of emergency helper software with broader functionality. The chatbot called Aiden is designed to impart CPR and First Aid knowledge using easily digestible, concise text messages. As patients continuously receive quick and convenient access to medical services, their trust in the chatbot technology will naturally grow. Healthcare chatbots can locate nearby medical services or where to go for a certain type of care. For example, a person who has a broken bone might not know whether to go to a walk-in clinic or a hospital emergency room.
I was impressed by how Ada could handle various customer interactions and provide them with relevant and reliable information. ProProfs Chat is a healthcare chatbot that helps me communicate with my patients and provide them with the best care possible. It allows me to answer their queries, book appointments, send reminders, collect feedback, and more.
The use of chatbots for healthcare has proven to be a boon for the industry in many ways. Medical chatbots provide necessary information and remind patients to take medication on time. Medisafe empowers users to manage their drug journey — from intricate dosing schedules to monitoring multiple measurements. Additionally, it alerts them if there’s a potential unhealthy interaction between two medications.
Ready to Integrate Conversational AI Chatbots in Your Healthcare Company?
Launching an informative campaign can help raise awareness of illnesses and how to treat certain diseases. Before flu season, launch a campaign to help patients prevent colds and flu, send out campaigns on heart attacks in women, strokes, or how to check for breast lumps. These campaigns can be sent to relevant audiences that will find them useful chatbots and healthcare and can help patients become more aware and proactive about their health. One study found that there was no effect on adherence to a blood pressure–monitoring schedule [39], whereas another reported a positive improvement medication adherence [35]. I am looking for a conversational AI engagement solution for the web and other channels.
This includes ensuring the confidentiality, integrity, and availability of PHI as it is collected, stored, and shared. Since the current free version of ChatGPT does not support (nor does it intend to support) services covered under HIPAA through accessing PHI, the use of ChatGPT in health care can pose risks to data security and confidentiality. A well-designed healthcare chatbot can plan appointments based on the doctor’s availability.
A chatbot can be defined as specialized software that is integrated with other systems and hence, it operates in a digital environment. This means, chatbots and the data that they process might be exposed to threat agents and might be a target for cyberattacks. Chatbots in healthcare industry are awesome – but as any other great technology, they come with several concerns and limitations. It is important to know about them before implementing the technology, so in the future you will face little to no issues. The issue of mental health today is as critical as ever, and the impact of COVID-19 is among the main reasons for the growing number of disorders and anxiety. According to Forbes, the number of people with anxiety disorders grew from 298 million to 374 million, which is really a significant increase.
- One area of particular interest is the use of AI chatbots, which have demonstrated promising potential as health advisors, initial triage tools, and mental health companions [1].
- This includes ensuring the confidentiality, integrity, and availability of PHI as it is collected, stored, and shared.
- Similarly, one can see the rapid response to COVID-19 through the use of chatbots, reflecting both the practical requirements of using chatbots in triage and informational roles and the timeline of the pandemic.
- According to Forbes, the number of people with anxiety disorders grew from 298 million to 374 million, which is really a significant increase.
Where there is evidence, it is usually mixed or promising, but there is substantial variability in the effectiveness of the chatbots. This finding may in part be due to the large variability in chatbot design (such as differences in content, features, and appearance) but also the large variability in the users’ response to engaging with a chatbot. Healthcare chatbots are AI-driven virtual assistants designed to interact with users in the healthcare domain.
Due to the small numbers of papers, percentages must be interpreted with caution and only indicate the presence of research in the area rather than an accurate distribution of research. With the chatbot remembering individual patient details, patients can skip the need to re-enter their information each time they want an update. This feature enables patients to check symptoms, measure their severity, and receive personalized advice without any hassle. Patients can book appointments directly from the chatbot, which can be programmed to assign a doctor, send an email to the doctor with patient information, and create a slot in both the patient’s and the doctor’s calendar. The chatbot has a user-friendly interface that helped me design my chatbot’s personality, appearance, and behavior. I could also choose from various characters, languages, and voice variations or create my own from scratch.
QuickBlox Releases One of the First HIPAA-Compliant Chatbots With OpenAI BAA – Newswire
QuickBlox Releases One of the First HIPAA-Compliant Chatbots With OpenAI BAA.
Posted: Wed, 27 Mar 2024 13:00:00 GMT [source]
While being seriously impacted by the COVID-19, the healthcare industry is steadily gaining traction in terms of its digital transformation and is adopting more and more innovative technologies on a regular basis. Chatbots, being among the most affordable solutions, have become valuable assets for healthcare organizations worldwide, and their value is recognized by both medical professionals and patients. Another challenge involves the data provided to ChatGPT in the form of user prompts. When users ask the tool to answer some questions or perform tasks, they may inadvertently hand over sensitive personal and business information and put it in the public domain. For instance, a physician may input his patient’s name and medical condition, asking ChatGPT to create a letter to the patient’s insurance carrier.
As technology improves, conversational agents can engage in meaningful and deep conversations with us. Case in point, people recently started noticing their conversations with Bard appear in Google’s search results. This means Google started indexing Bard conversations, raising privacy concerns among its users. So, despite the numerous benefits, the chatbot implementation in healthcare comes with inherent risks and challenges. Our tech team has prepared five app ideas for different types of AI chatbots in healthcare. A thorough research of LLMs is recommended to avoid possible technical issues or lawsuits when implementing a new artificial intelligence chatbot.
The Physician Compensation Report states that, on average, doctors have to dedicate 15.5 hours weekly to paperwork and administrative tasks. With this in mind, customized AI chatbots are becoming a necessity for today’s healthcare businesses. The technology takes on the routine work, allowing physicians to focus more on severe medical cases. Chatbots in the healthcare industry provide support by recommending coping strategies for various mental health problems. Most chatbots (we are not talking about AI-based ones) are rather simple and their main goal is to answer common questions. Hence, when a patient starts asking about a rare condition or names symptoms that a bot was not trained to recognize, it leads to frustration on both sides.
Penjarahan Barang Antik Telah Meningkat di Bawah Lockdown – Selain menyebabkan kekacauan dan kesengsaraan bagi sebagian besar orang, krisis pandemi COVID-19 telah memperluas peluang penjarahan, pencurian, dan perdagangan gelap salah satu sumber daya terpenting dunia warisan budayanya.

Ketidakstabilan Sosial
Ketidakstabilan sosial dan tekanan keuangan dapat bergabung untuk mendorong penjarahan situs arkeologi di seluruh dunia, khususnya di Timur Tengah dan Afrika Utara, memberi makan pasar gelap online global dalam perdagangan barang antik, yang diperkirakan memiliki omset harian sebesar US$10 juta (£ 7,9 juta). https://hari88.com/
Ada bukti signifikan bahwa kelompok teroris seperti Negara Islam mendapat keuntungan dari perdagangan pasar gelap barang antik yang dijarah dari Irak dan Suriah.
Sebuah negara yang telah mengalami episode perusakan berulang dari penjarahan situs dan koleksi museum adalah Irak. Pada tahun 1991, 2003 dan 2014-17, situasi konflik dan krisis telah mendorong penggeledahan dan pencurian aset warisan Irak yang tak ternilai.
Yang paling terkenal, pada April 2003 setelah invasi pimpinan AS/Inggris ke Irak, Museum Irak di Baghdad kehilangan ribuan kepingnya yang paling berharga, banyak di antaranya tidak pernah ditemukan kembali.
Warisan budaya Irak, tempat saya bekerja sebagai arkeolog selama lebih dari 35 tahun, memiliki signifikansi nasional dan global. Beberapa desa pertanian pertama di dunia, kota dan tulisan pertama di dunia, dan kerajaan awal semuanya dikembangkan oleh komunitas di tanah Irak, Mesopotamia kuno.
Perlindungan Dan Promosi Warisan Irak
Sebagai presiden RASHID Internasional (Penelitian, Penilaian dan Perlindungan Warisan Irak dalam Bahaya), saya bekerja sama dengan rekan-rekan Irak dan internasional untuk meningkatkan perlindungan dan promosi warisan Irak, menempatkannya dalam kerangka hak budaya yang mempromosikan akses yang adil ke dan kenikmatan situs warisan dan aset oleh semua komunitas Irak.
Bekerja sama dengan rekan-rekan dari University of Reading dan didukung oleh hibah dari British Council’s Cultural Protection Fund, kami baru-baru ini menyelesaikan proyek ambisius untuk meningkatkan keamanan dan perlindungan lebih dari 270.000 artefak tak ternilai dalam koleksi Museum Irak di Baghdad dan Slemani Museum di Sulaimaniyah di wilayah Kurdistan Irak.
‘Ketertelusuran cair’
Untuk melakukan ini, kami menggunakan produk komersial, SmartWater, yang bekerja dengan memberikan “ketertelusuran cair” ke objek dan material yang dilindungi. Dengan menerapkan titik kecil atau semprotan cairan “pintar” ke artefak dalam koleksi museum, menjadi mungkin untuk membuktikan sumber museum dari setiap objek, jika mereka dipindahkan secara ilegal dari museum tuan rumah mereka.
Setiap titik cairan berisi kode unik khusus untuk museum itu. Cairan tidak terlihat dengan mata telanjang tetapi bersinar terang di bawah sinar UV langsung. Uji tuntas telah menetapkan daya tahan dan kurangnya efek negatif bila diterapkan pada benda-benda dari bahan anorganik, seperti tembikar, batu, kaca dan logam.
Sejak cairan ini dikembangkan pada awal 1990-an, lebih dari satu juta bisnis, rumah, dan bangunan bersejarah di seluruh dunia telah mengadopsinya.
Dua tujuan utama penandaan artefak dengan cara ini adalah pencegahan dan ketertelusuran. Setelah menandai benda-benda di museum, papan nama yang terlihat jelas dipajang di museum, sebagai sarana untuk mencegah pencurian.
Elemen Pencegahan
Studi di Inggris menunjukkan bahwa hingga 74% penjahat menahan diri dari melakukan kejahatan pencurian di mana tanda-tanda perusahaan ditampilkan. Elemen pencegahan masuk ke pasar gelap, memperkenalkan risiko dan mengurangi selera pembeli potensial dan saluran seperti rumah lelang.
Tetapi jika benda-benda yang dilindungi dicuri, sebuah penelitian menunjukkan bahwa keterlacakan cairan yang dikodekan berarti bahwa benda-benda itu dapat dilacak secara permanen, dan dapat dipulangkan ke rumah yang tepat begitu mereka ditemui dalam situasi seperti penjualan rumah lelang dan katalog dan di forum online.
Menandai waktu
Didukung oleh hibah sebesar £156.000 dari Cultural Protection Fund, pada tahun 2019 saya memimpin tim rekan kerja, termasuk Dr Amy Richardson dan Ali Al-Makhzoomi di University of Reading, Phil Cleary di SmartWater Foundation, dan direktur serta staf Museum Irak dan Museum Slemani di Irak, dalam penerapan SmartWater untuk artefak dalam koleksi mereka.
Bekerja dengan jadwal yang ketat, tim berhasil menerapkan solusi cair ke total 273.000 objek di kedua museum. Benda-benda yang dirawat termasuk bejana tembikar, peralatan batu, koin logam dan perhiasan dan ornamen kaca, dari seluruh rentang warisan kaya Irak. Semua artefak ini sekarang dapat dilacak secara permanen sebagai milik museum masing-masing.
Lebih penting lagi, melalui proyek ini kami melatih total 43 profesional museum Irak tentang protokol penggunaan teknologi untuk melindungi koleksi mereka. Para profesional ini sekarang dalam posisi untuk menularkan keterampilan dan keahlian mereka kepada rekan-rekan baik di dalam maupun di luar institusi mereka sendiri.
Melihat ke masa depan, di University of Reading kami bekerja sama dengan rekan-rekan SmartWater dalam pengembangan larutan cair yang cocok untuk aplikasi pada objek museum yang terbuat dari bahan organik seperti kain, kertas, kulit, dan kayu.

Kami juga menjajaki perluasan proyek untuk mencakup museum lain di Irak dengan koleksi yang rentan, dan koleksi museum di wilayah lain di dunia.
Salah satu negara tersebut adalah Yaman, di mana ketidakstabilan dan konflik yang sedang berlangsung menghasilkan peluang untuk eksploitasi gelap salah satu sumber daya terbesar dunia warisan arkeologi dan sejarahnya.
Pecinta Sappho Senang Dengan Penemuan Puisi ‘Baru’ – Museum of the Bible di Washington baru-baru ini mengumumkan telah mengembalikan 5.000 fragmen papirus kuno ke Mesir. Di antaranya adalah fragmen puisi penyair Yunani kuno Sappho yang diperoleh museum pada 2012.

Asal Usul Fragmen
Pengumuman tersebut mengikuti pertanyaan bertahun-tahun tentang asal-usul fragmen, dan asal-usul fragmen dari gulungan papirus yang sama yang menjadi perhatian publik pada tahun 2014. Para sarjana dan kritikus sastra beramai-ramai setelah The Daily Beast melaporkan pada 28 Januari 2014, bahwa ahli papyrologi Dirk Obbink dari Universitas Oxford telah mengidentifikasi dua puisi baru karya Sappho. premium303
Sappho of Lesbos adalah salah satu penyair lirik Yunani paling awal, terkenal di zaman kuno karena polesan dan keanggunan syairnya.
Hari ini, warisan Sappho melampaui puisi. Ekspresi hasratnya terhadap sesama jenis (“… keringat mengalir di tubuhku / getaran mengguncangku …”) telah membuatnya menjadi ikon bagi beberapa komunitas LGBTQ+.
Hanya sedikit puisi Sappho yang bertahan, dan yang terjadi hanyalah terpisah-pisah. Penemuan Obbink sangat luar biasa karena mempertahankan lima bait terakhir dari satu puisi dan bagian dari satu detik, menjadikannya salah satu urutan syair Sapphic yang terpanjang.
Berita penemuan itu menjadi berita utama internasional, tetapi pertanyaan serius tentang asal- usul, akuisisi, dan sejarah kepemilikan papirus asalnya tidak. Asalnya penting untuk menetapkan keaslian dan status hukum barang antik.
Penelitian Baru
Pada musim gugur, saya menerbitkan penelitian baru tentang brosur penjualan digital yang diproduksi oleh rumah lelang Christie’s. Penelitian saya mempertanyakan laporan yang diterbitkan tentang asal papirus.
Saya percaya bahwa catatan tentang asal usul papirus Sappho yang diterbitkan Obbink adalah palsu, dan bahwa pemiliknya memiliki akses ke penelitian Obbink yang tidak dipublikasikan dan berusaha memanfaatkannya.
Masalah hukum dan etika
Papirus berasal hampir tanpa kecuali di Mesir. Pada tahun 1983, pemerintah Mesir mengeluarkan undang-undang yang melarang perdagangan barang antik dalam negeri, menetapkan secara definitif bahwa warisan arkeologi negara itu adalah milik negara.
Untuk memerangi penjarahan dan perdagangan barang antik ilegal, lebih dari satu pedoman etika asosiasi ilmiah mengutip Konvensi UNESCO 1970 tentang Kekayaan Budaya dalam mengutuk studi barang antik yang baru muncul.
Menurut pedoman itu, para cendekiawan tidak boleh mengotentikasi atau mempublikasikan benda-benda yang meninggalkan negara asalnya secara ilegal atau sebelum konvensi 1970. Bagaimana dan kapan papirus Sappho meninggalkan Mesir menimbulkan pertanyaan hukum dan etika.
The Daily Beast ditautkan ke artikel draf yang tidak dipublikasikan Obbink tersedia secara singkat di blog. Mengenai asal-usul papirus, dikatakan hanya bahwa itu baru ditemukan dan dalam koleksi pribadi pemilik anonim.
Pertanyaan ilmiah
Sejarawan dan penyiar Bettany Hughes segera melaporkan di London’s Sunday Times bahwa Obbink menemukan papirus setelah mengambilnya dari karton mumi casing pemakaman Mesir yang mirip dengan papier-mâché.
Obbink menguatkan asalnya dalam karton mumi dalam artikel Suplemen Sastra Times.
Hughes menyatakan bahwa “asal dari papirus itu tidak jelas” dan bahwa “awalnya tampaknya dimiliki oleh seorang perwira tinggi Jerman.” Obbink hanya mengatakan bahwa asalnya didokumentasikan dan legal.
Narasi Mumi Karton
Para sarjana mempertanyakan narasi mumi karton karena praktik daur ulang papirus dalam pembuatan karton berhenti jauh sebelum papirus disalin.
Ketika makalah ilmiah Obbink akhirnya diterbitkan pada 10 April 2014, itu tidak membahas asalnya.
Setahun kemudian, Obbink merevisi cerita asal papirus pada konferensi ilmiah pada 9 Januari 2015. Dia mengatakan itu ditemukan dari fragmen karton papirus yang tidak dicat yang dibeli di lelang Christie’s 2011. Dia tidak merinci kapan pemulihan itu terjadi.
Brosur Christie
Setelah presentasi Obbink, Christie’s mengeluarkan brosur 26 halaman yang mengiklankan papirus Sappho baru untuk penjualan pribadi. Itu beredar secara eksklusif di antara klien Christie, dan tidak diketahui oleh para sarjana.
Saya menerima salinan digital dari Ute Wartenberg Kagan, seorang sarjana mata uang Yunani kuno, yang diperolehnya dari klien Christie’s. Brosur itu berisi foto-foto yang diberi judul “pemulihan papirus Sappho.”
Ketika saya menanyakan tentang brosur tersebut, Christie’s menjawab: “Kami tidak dapat mendiskusikan aktivitas penjualan pribadi kecuali jika diizinkan untuk melakukannya.”
Saya berharap untuk mengetahui kapan file-file itu dibuat dan dimodifikasi, dan untuk meneliti lebih dekat apa yang digambarkan oleh gambar-gambar itu. Saya menjalankan program komputer yang memeriksa brosur dan file JPG-nya, dan dapat mengekstrak metadata yang terkait dengannya.
Brosur Christie
Saya menyimpulkan bahwa foto-foto yang disajikan dalam brosur Christie adalah rekayasa dan tidak menggambarkan ekstraksi papirus Sappho.
Dalam pandangan saya, foto-foto tersebut mendokumentasikan cerita tentang karton mumi yang ditulis oleh Hughes dan Obbink.
Satu foto termasuk panel karton yang saya identifikasi sebelumnya milik seorang perwira tinggi Jerman, seperti yang disebutkan dalam laporan Hughes. Kisah itu tidak pernah masuk akal para sarjana mempertanyakannya dan Obbink kemudian merevisinya. Tetapi brosur itu, saya yakin, menjadi saksi dari narasi aslinya.
Penelitian Obbink
Saya juga menyimpulkan bahwa pemilik anonim dari papirus memiliki akses ke penelitian Obbink yang tidak dipublikasikan, dan mulai mengusulkan papirus untuk penjualan pribadi segera setelah Obbink mempresentasikan cerita yang direvisi pada konferensi ilmiah 9 Januari 2015.
Bagian “Asal usul” brosur tidak mengutip presentasi Obbink pada bulan Januari tetapi artikel ilmiah yang tidak diterbitkan sampai 15 Juni, hampir empat bulan setelah pembuatan brosur.
Menanggapi sebuah artikel di The Guardian yang melaporkan penelitian saya, Christie’s mengatakannya: “… tidak akan pernah dengan sengaja menawarkan karya seni apa pun tanpa judul yang bagus atau katalog atau otentikasi yang salah.
Kami menganggap nama dan reputasi kami dengan sangat serius dan akan mengambil semua langkah yang diperlukan yang tersedia untuk mengatasi situasi penggunaan yang tidak pantas.”
Etika ilmiah dan barang antik
Para sarjana waspada terhadap pasar barang antik karena penilaian akademis menambah nilai komersial objek, yang dapat mendorong penjarahan dan perdagangan ilegal barang antik. Beasiswa juga menawarkan legitimasi.
Untuk itu, para sarjana harus meneliti penemuan-penemuan baru dengan cermat sebelum melakukan atau mempublikasikan penelitian, dan mempresentasikan temuannya secara transparan. Ketika media melaporkan penelitian pendahuluan, penting untuk menyampaikan sifat awalnya.

April lalu, sebuah surat kabar mahasiswa Oxford melaporkan bahwa Obbink telah ditangkap pada 2 Maret 2020, karena “dugaan pencurian papirus kuno dari Sackler Classics Library di Oxford”. Obbink telah membantah tuduhan itu.
Saatnya Merayakan Pemburu Fosil Afrika Yang Terlupakan – Ada beberapa hal yang lebih menarik bagi ahli paleontologi profesional daripada menemukan sisa-sisa fosil. Pada awal 2017 saya menemukan kerangka yang diawetkan dengan indah mencuat dari tanah di wilayah Karoo, Afrika Selatan. Itu adalah tulang punggung hewan herbivora besar yang disebut pareiasaur.

Lengkungan vertebral individu disertai oleh dua bilah pinggul hewan itu. Fragmen kaki depannya dan beberapa bagian tengkoraknya juga terlihat. Semua ini menunjukkan bahwa saya telah menemukan kerangka hampir 2 meter, sisanya tersembunyi di bawah tanah. Fosil berusia 275 juta tahun ini tidak memiliki kelainan bentuk dan mudah diidentifikasi. https://www.premium303.pro/
Saya menyadari bahwa bahkan seseorang yang tidak terlatih dalam paleontologi akan dengan mudah menemukan tulang yang terkikis dan mengenalinya sebagai sisa-sisa makhluk raksasa.
Ini membuat saya berpikir tentang pencari fosil paling awal di Afrika, yang identitasnya sebagian besar tidak diketahui. Siapa mereka, dan bagaimana penemuan mereka memengaruhi pemikiran kita tentang evolusi? Berapa banyak ide mereka yang ditolak atau dihapus dari sejarah setelah kedatangan kolonialisme dan pemburu fosil barat di benua itu?
Sangat penting untuk menghormati orang-orang ini dan penemuan fosil mereka, yang merupakan contoh dari warisan budaya dan paleontologi.
Perburuan fosil bersejarah di Afrika
Bagi banyak orang, sejarah penemuan fosil tulang di Afrika tidak dapat dipisahkan dari ekspedisi terkenal yang dipimpin oleh Eropa. Banyak dari ini terjadi selama abad ke-19 dan ke-20 dan menjadi berita utama yang membuat sesak napas di seluruh dunia.
Ada ekspedisi Jerman di Tendaguru (Tanzania), yang menghasilkan kerangka luar biasa dari beberapa dinosaurus terbesar yang pernah ditemukan. Ahli paleontologi Amerika dan Eropa juga melakukan beberapa perjalanan ke depresi Fayum di Mesir karena itu adalah rumah bagi mamalia dari segala jenis dan ukuran sekitar 35 juta tahun yang lalu.
Ekspedisi ini menangkap imajinasi publik. Tetapi catatan arkeologi mengungkapkan bahwa fosil ditemukan dan dikumpulkan jauh sebelum perjalanan semacam itu , oleh para amatir yang menggunakannya, misalnya, dalam ritual keagamaan.
Dalam bukunya tentang penemuan fosil di zaman klasik, “The First Fossil Hunters”, Adrienne Mayor menyebutkan bahwa tulang-tulang raksasa ditemukan di Maroko pada awal 300 hingga 400 SM. Dia menduga itu adalah fosil gajah.
Salah satu penemuan fosil kuno paling terkenal di Afrika melibatkan gigi raksasa. Teolog dan filsuf Kristen Saint Augustin, uskup yang sekarang bernama Aljazair, menemukannya di dekat Utica (Tunisia) pada abad keempat M. Ini terbukti sebagai fosil geraham gajah.
Namun, penemuan Saint Augustin bukanlah contoh koleksi fosil tertua di Afrika. Gelar itu diberikan kepada orang Mesir kuno yang mengumpulkan dan mengumpulkan tulang fosil mamalia berusia jutaan tahun dan mengemasnya dalam kain linen, kemungkinan sebagai bentuk pemujaan kepada Set.
Kolektor fosil ini hidup 3000 tahun yang lalu. Ada juga bukti fosil gigi hiu yang dikumpulkan dan ditusuk untuk dipakai sebagai liontin di Mesir kuno, sekitar 6500 tahun yang lalu.
Pencarian kolektor fosil pertama
Ada kemungkinan bahwa fosil dikenali di Afrika lebih awal dari ini. Di Kongo, sebuah situs yang berusia 21.000 tahun telah menghasilkan gigi fosil gajah yang punah jutaan tahun sebelumnya. Ini menunjukkan bahwa seseorang menemukan fosil gigi besar ini dan membawanya pulang, mungkin sebagai barang antik.
Selain itu, situs seni cadas Khoisan yang tidak bertanggal di Lesotho tampaknya mewakili jejak kaki dinosaurus. Jejak fosil yang berasal dari lebih dari 200 juta tahun yang lalu tidak jarang ditemukan di wilayah ini, dan sering terekspos dengan baik terletak dekat dengan permukaan bumi sehingga masuk akal jika penduduk kuno telah melihat dan mendokumentasikannya. Khoisan bisa jadi adalah orang pertama yang menemukan fosil di Afrika Selatan.
Meskipun hipotesis ini masih diperdebatkan dengan hangat, gambar-gambar ini disertai dengan lukisan gua yang menunjukkan bahwa Khoisan menafsirkan jejak kaki ini sebagai milik ras burung raksasa yang tidak bisa terbang.
Saat ini, sebagian besar ilmuwan menganggap burung sebagai kerabat terdekat dinosaurus. Ini menyiratkan bahwa nenek moyang orang Khoisan memiliki pemahaman yang luar biasa tentang rekonstruksi ilmiah, meskipun belum ada kerangka evolusi yang dijelaskan.
Sebelum Darwin
Khoisan bukan satu-satunya orang di Afrika yang berpikir jauh di depan kurva Darwinian. Sejumlah cendekiawan Muslim dari Timur Tengah dan Afrika Utara membuat pernyataan yang sangat eksplisit dan berpandangan jauh ke depan berabad-abad sebelum Darwin.
Misalnya, seorang cendekiawan Tunisia bernama Ibn Khaldun, menyatakan sejak tahun 1377 bahwa “tingkat manusia yang lebih tinggi dicapai dari dunia monyet, di mana kecerdasan dan persepsi ditemukan.”
Dia mungkin terinspirasi oleh pendahulunya, Persia Ibn Miskawaih (932-1030), yang menyatakan dalam Brothers of Purity bahwa “Hewan […] akhirnya mencapai perbatasan kemanusiaan dengan Kera yang hanya satu derajat di bawah Manusia dalam skala dari evolusi”.
Sangat mungkin bahwa Darwin tidak tahu tentang penemuan kuno dan penulis abad pertengahan ini karena mereka tidak disebutkan dalam biografi atau karyanya. Tetapi fakta bahwa mereka ada menggambarkan potensi besar Afrika untuk mempengaruhi dan mengembangkan penelitian paleontologi.

Tantangannya sekarang adalah untuk membangun warisan ini dan meningkatkan kesadaran tentang penemuan dan teori yang telah lama terlupakan ini. Ini adalah cara penting untuk memotivasi generasi baru peneliti fosil Afrika.
Perdagangan Yang Ilegal Dalam Barang Antik – Penjarahan artefak selalu menjadi tanda kekuatan militer atau kekuatan ekonomi. Selama ribuan tahun, para jenderal penakluk akan membawa serta piala untuk menghiasi kota mereka.
Di abad yang lebih baru, kelas atas yang kaya akan melakukan “tur besar” ke situs klasik dan memperoleh dengan cara apa pun apa pun mulai dari vas hingga patung hingga seluruh dekorasi kuil untuk dipamerkan di rumah.
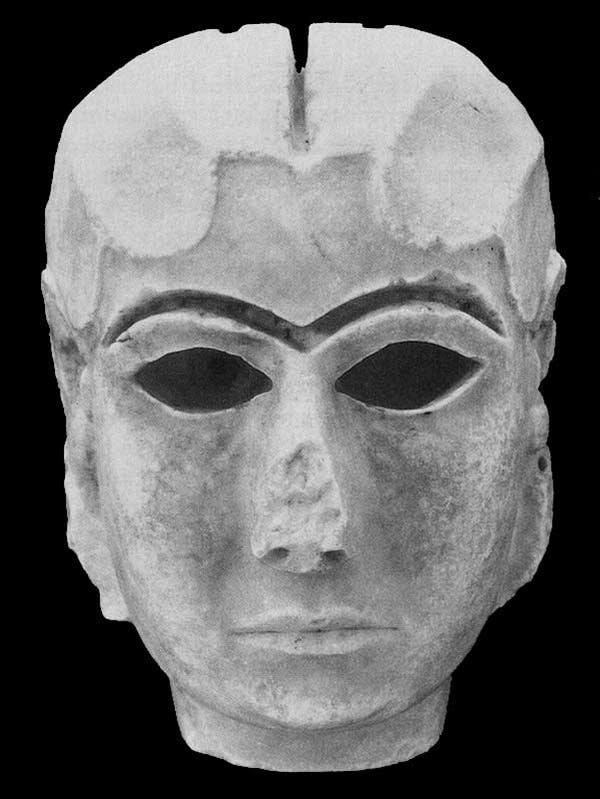
Memiliki sepotong barang antik dipandang sebagai menunjukkan kekayaan, kecintaan pada budaya kuno dan, pada akhirnya, perbedaan seseorang: memiliki hal-hal yang tidak dapat dimiliki orang lain. hari88
Bentuk Koleksi
Setidaknya inilah yang dipikirkan para penjarah. Sekarang kita semua harus tahu cara paling tepat untuk menggambarkan bentuk koleksi yang meragukan ini – dan itu adalah kata yang memiliki resonansi historis: vandalisme.
Begitu banyak barang antik dicuri sehingga memenuhi museum kekaisaran besar di banyak ibu kota dunia: museum Inggris, Louvre, Metropolitan, museum Istanbul. Lembaga-lembaga ini terus memegang harta nasional negara lain, mengklaim bahwa mereka adalah museum internasional yang menyimpan warisan dunia dan membuatnya tersedia untuk semua orang.
Begitu pula dengan Parthenon Marbles salah satu tindakan vandalisme paling kontroversial dari semuanya diadakan di British Museum di London setelah “diakuisisi” secara meragukan oleh Thomas Bruce, Earl of Elgin pada tahun 1801, kurang dari tiga dekade sebelum kemerdekaan Athena dari pemerintahan Ottoman.
Pemimpin oposisi Inggris, Jeremy Corbyn, baru-baru ini menyatakan bahwa pemerintah Partai Buruh akan mengembalikan kelereng ke Yunani. Dalam sebuah pernyataan pada 3 Juni dia berkata:
“Seperti apapun yang dicuri atau diambil dari pendudukan atau kepemilikan kolonial termasuk artefak yang dijarah dari negara lain di masa lalu – kita harus terlibat dalam pembicaraan konstruktif dengan pemerintah Yunani tentang pengembalian patung”
Posisi tradisional pemerintah Inggris pada kelereng Parthenon adalah terserah pada pengurus British Museum untuk memutuskan pengembalian artefak dalam koleksinya. Tapi, karena pemerintah adalah penyandang dana utama museum, hal itu pasti dapat memberikan pengaruh yang kuat pada keputusan pengawas.
Jadi kelereng tetap ada di London. Dan perdagangan barang antik masih kuat tidak hanya merampas warisan negara-negara mereka, tetapi, yang lebih buruk, merampas informasi dunia yang dapat diekstraksi dengan penggalian sistematis yang tepat dan mengurangi artefak menjadi karya seni belaka yang hanya dapat dinikmati dalam konteks museum yang basi dan bukan sebagai gejala yang kaya dan guru sejarah umat manusia.
Sementara itu, terdapat bukti bahwa pendapatan dari penjualan barang antik curian yang dijarah di Suriah dan Irak telah digunakan untuk mendanai ISIS dan kelompok teroris lainnya jadi satu aktivitas ilegal telah dikaitkan dengan banyak aktivitas lainnya.
Memerangi perdagangan
Bagaimana kita menghentikan perdagangan yang merupakan momok pengetahuan sejarah, kebanggaan lokal dan kedaulatan internasional ini. Perdagangan barang antik terlarang dan hampir semua perdagangan barang antik adalah ilegal dalam arti tertentu, karena hampir selalu melanggar hukum negara asal dianggap sebagai kejahatan umum.
Di banyak negara ada departemen kepolisian yang mengkhususkan diri pada jenis kejahatan ini. Misalnya, Inggris Raya memiliki unit seni dan barang antik Kepolisian Metropolitan dan di AS FBI memiliki Tim Kejahatan Seni yang beranggotakan 16 orang.
Di Inggris, “Operation Bullrush” oleh unit seni dan barang antik berhasil menuntut dealer Jonathan Tokeley-Parry pada tahun 1997 karena menyelundupkan barang antik yang tak ternilai harganya ke luar Mesir (dia juga dijatuhi hukuman in absentia di Mesir).
Sementara itu pada tahun 2002 pengadilan AS menghukum Frederick Schultz, mantan presiden Asosiasi Nasional Dealer Seni Kuno, Oriental dan Primitif, di bawah Undang-Undang Properti yang Dicuri Nasional (NSPA) 1934 atas konspirasi untuk menerima barang antik yang dicuri dari Mesir.
Sementara itu, berbagai negara sedang menandatangani nota kesepahaman (MOU) untuk mengendalikan impor barang antik dan mengkoordinasikan upaya pencegahan penyelundupan. Pada 2017, AS menyelesaikan MOU dengan Mesir.
Pengaturan ini didukung oleh konvensi Paris UNESCO tahun 1970 yang melarang penjualan dan pembelian seni kuno yang belum beredar sebelum ratifikasi perjanjian itu oleh masing-masing negara.
Tetapi sebagian besar tindakan dan pemangku kepentingan ini berfokus pada tujuan akhir dari barang antik terlarang, kolektor atau museum – dan ini tidak cukup.
Perlu ada tindakan untuk memperhitungkan semua tahap perdagangan barang antik ilegal: dari penggalian ke perantara pertama dan kedua (dealer), hingga mereka yang mengangkutnya dari satu negara ke negara lain, ke pembeli akhir, kolektor.
Bekerja bersama
Organization Heritage Manajemen (HERITΛGE), sebuah proyek yang terkait dengan University of Kent, telah bekerja untuk menciptakan strategi yang komprehensif untuk perdagangan barang antik terlarang, yang bertujuan untuk menggabungkan pengetahuan dan upaya dari berbagai pemangku kepentingan: ilmuwan, masyarakat setempat, polisi, kolektor, legislator dan masyarakat.
Untuk mencegah penggalian ilegal, pasukan polisi perlu menggunakan kemajuan teknologi terbaru seperti pengawasan satelit, pengenalan pola, dan ilmu forensik.
Tetapi mereka membutuhkan bantuan dari komunitas lokal di area arkeologi yang perlu menjadi lebih positif sebagai pemangku kepentingan dalam perlindungan warisan mereka.
Para kolektor tidak boleh dilihat semuanya sebagai musuh tetapi sebagai pemangku kepentingan yang berpotensi kuat yang perlu dilibatkan dan dilatih dalam memerangi perdagangan barang antik ilegal. Banyak kolektor berhati-hati dalam cara membeli tetapi yang lain tidak tahu cara membeli dengan lebih bertanggung jawab.
Para kolektor memiliki wawasan dan informasi berharga tentang jaringan klandestin, pedagang barang seni dan verifikasi yang berpotensi ketat (atau tidak) dari status hukum masing-masing bagian dalam koleksi mereka sendiri.
Dengan kerja sama Kementerian Kebudayaan Yunani, HERITΛGE menyelenggarakan pertemuan pertama antara kolektor, kementerian, dan polisi di Yunani. Masih banyak yang harus dilakukan di bidang ini.
Sangat baik memiliki perjanjian internasional untuk mengontrol perdagangan barang antik, tetapi pertama-tama perjanjian itu harus dipahami oleh semua pemangku kepentingan terkait. HERITΛGE telah menerbitkan satu dari sedikit komentar tentang restitusi di Hukum Eropa dan internasional.

Relawan sangat penting untuk dilatih tentang cara memeriksa asal barang yang akan dijual dan tentang cara menggunakan database yang ada untuk “menangkap” barang klandestin atau barang curian. Salah satu contohnya adalah akademisi Christos Tsirogiannis yang telah berhasil melacak barang antik yang dijarah dan memastikan mereka dikembalikan ke negara asalnya.
Tapi, agar strategi ini membuahkan hasil, semua pemangku kepentingan yang relevan perlu berkolaborasi dengan pikiran terbuka dan kemudian mungkin ada kemungkinan bahwa kita akan dapat mengakhiri ribuan tahun perusakan warisan nasional begitu banyak negara.
Koin Terlangka dan Paling Berharga di Dunia Bagian 2 – Terkadang, permen membuat koin yang sangat tidak biasa sebagai aksi pemasaran dengan tujuan tidak akan pernah dijual.
Misalnya, Koin Emas Satu Ton Kanguru Australia yang dibuat oleh Perth Mint di Australia pada tahun 2011. Setelah tur publisitas di Eropa, koin tersebut sekarang dipajang secara permanen di Pameran Emas The Perth Mint.

Kanada juga membuat koin emas yang sangat besar, sebagian besar untuk publisitas, tetapi mereka menjual lima di antaranya ke berbagai investor dan kolektor. https://3.79.236.213/
Selain itu, hanya koin yang diperdagangkan secara publik (misalnya, lelang atau penjualan publik) yang terdaftar. Tidak mungkin untuk memverifikasi koin yang dijual melalui perjanjian pribadi dan oleh karena itu tidak termasuk dalam daftar teratas dari koin paling berharga di dunia ini. Berikut ini beberapa koin paling berharga di dunia.
1913 Liberty Head Nickel – Morton-Smith-Eliasberg Specimen
Spesimen nikel Kepala Liberty 1913 ini sejauh ini merupakan contoh terbaik dari hanya lima spesimen. Spesimen Koleksi Dr. William Morton-Smith / Louis E. Eliasberg, Sr. dilelang pada Agustus 2018 di ANA US Coins Auction di Philadelphia, PA.Spesimen ini memiliki permukaan yang sangat mirip cermin di lapangan.
Ini adalah satu-satunya koin dari lima koin yang menunjukkan karakteristik ini. Karena tidak ada catatan pencetakan yang ada untuk produksi koin ini, menyebabkan beberapa kontroversi. Ini telah dinilai oleh perata koin profesional yang bervariasi dari MS-62 Proof-64.
1787 Brasher Doubloon – EB on Breast
Meskipun koin ini tidak dijual di pelelangan koin, Blanchard and Company menempatkannya ke tangan seorang kolektor pribadi seharga lebih dari $ 7.000.000. Berbeda dengan Brasher Doubloon (# 4) tahun 1787 sebelumnya yang memiliki cap counter Ephraim Brasher di sayap elang, koin ini bertanda di dada elang.
Koin itu dicetak pada tahun 1787 oleh Ephraim Brasher, seorang pengrajin perak dan pandai emas di New York City, dan pada saat itu mengandung emas senilai $ 15.
Brasher juga membuat sejumlah kecil koin emas yang kami yakini dimaksudkan untuk peredaran publik karena US Mint belum mulai beroperasi.
1787 Brasher Doubloon – EB on Wing
Ephraim Brasher adalah seorang pandai emas dan perak di daerah New York City pada akhir tahun 1700-an. Karena United States Mint belum beroperasi, koloni terpaksa mencetak koin mereka sendiri.
Pengusaha swasta seperti Brasher mencetak beberapa koin ini. Banyak numismatis, termasuk tokoh terkenal seperti Henry Chapman dan Q. David Bowers, mengakui Brasher Doubloon sebagai koin terpenting di dunia.
Brasher membuat dobloon Brasher Gaya New York pada tahun 1787, dan spesifikasi untuk koinnya hampir identik dengan Lima dobloon dan sangat mirip dengan koin-koin Spanyol sebelumnya pada periode itu.
1933 Double Eagle
Pada tahun 1933, Amerika Serikat berada di tengah-tengah. Hampir 500.000 dua puluh dolar keping emas dicetak pada tahun itu. Presiden Roosevelt mengeluarkan perintah eksekutif untuk menarik semua koin emas dari masyarakat umum dan memerintahkan mint untuk melebur semua keping emas senilai $ 20 yang masih dimilikinya.
Entah bagaimana, segelintir tahun 1933 yang bertanggal $ 20 keping emas lolos dari brankas mint meskipun tidak pernah dikeluarkan secara resmi. Saat ini mereka ilegal untuk dimiliki dan akan disita oleh pemerintah Amerika Serikat.
Kecuali satu, yang pada awalnya dimiliki oleh Raja Farouk dari Mesir. Setelah pertarungan hukum yang panjang, Mint dan pemilik pribadi setuju untuk menjual koin dan membagi hasilnya. Pembeli harus membayar tambahan $ 20 kepada mint untuk memonetisasi koin sehingga ilegal untuk dimiliki.
1794 Flowing Hair Silver Dollar
Dijual oleh perusahaan lelang Stack’s Bowers di New York Americana Sale bulan Januari 2013 , koin ini menetapkan rekor dunia untuk penjualan satu koin. Peneliti numismatik percaya itu adalah dolar perak pertama yang pernah dicetak oleh Amerika Serikat.
United States Mint pertama kali dibuka pada tahun 1792, dan hanya mencetak koin tembaga dan beberapa koin pola selama dua tahun pertama. Kolektor koin telah mempertahankan contoh murni ini dalam kondisi asli mintnya selama lebih dari 200 tahun. Jarang sekali Anda menemukan koin setua ini dan dalam kondisi hampir sempurna.
Dari seluruh populasi yang diketahui dari 1794 dolar perak, ini adalah satu-satunya contoh yang menunjukkan reflektifitas seperti Bukti di lapangan.

Jika dilihat dari enkapsulasinya, bidang berkedip dengan pantulan cermin dalam yang mencengangkan, memberikan kontras yang luar biasa ke perangkat yang sepenuhnya buram. Beberapa dolar perak 1795 memiliki colokan perak tetapi juga menunjukkan tanda penyesuaian.
Pada koin ini, tanda penyesuaian ringan tetapi dicatat pada bagian depan dan belakang, terutama di sekitar tepi. Istilah “kesempatan sekali seumur hidup” terlihat sekarang dan lagi, tetapi untuk bagian ini, itu sangat relevan, menurut siaran pers oleh Galeri Bowers Stack.
Koin Terlangka dan Paling Berharga di Dunia Bagian 1 – Ada banyak cara untuk menentukan nilai suatu barang. Cara terbaik untuk menentukan nilai koin adalah dengan meneliti koin yang sebenarnya dijual dan mencatat harga yang mereka realisasikan.
Beberapa koin adalah unik, disimpan di museum dan tidak akan pernah tersedia untuk dijual kepada masyarakat umum.
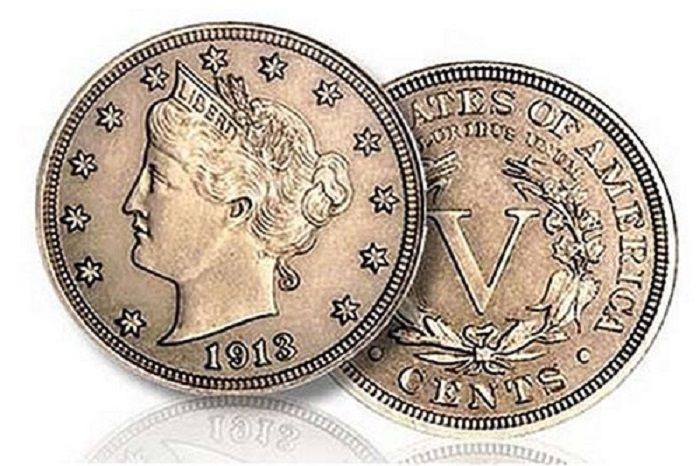
Karena koin-koin ini dianggap “tak ternilai”, mereka tidak termasuk dalam daftar koin paling berharga di dunia ini. Semua harga yang tercantum dalam dolar AS dan termasuk biaya lelang dan komisi yang dibebankan oleh rumah lelang kepada pembeli. www.mustangcontracting.com
1913 Liberty Head Nickel – Hawaii Five-O Star
Para peneliti secara luas percaya bahwa lima koin Liberty Head 1913 disambar oleh seorang karyawan mint di tengah malam. Mereka tidak yakin bagaimana koin mati untuk nikel Kepala Liberty 1913 dibuat sejak Buffalo Nickels pertama kali diproduksi pada tahun 1913. Namun, lima dari koin ini menemukan jalan mereka ke dalam berbagai koleksi koin publik dan pribadi.
Membintangi salah satu serial televisi tahun 1970-an Hawaii Five-O rupanya tidak membantu koin ini meningkat nilainya. Koin ini digunakan untuk bidikan close-up untuk acara televisi, sementara produser menggunakan nikel Liberty Head yang umum untuk pengambilan gambar aksi di mana tanggalnya tidak dapat ditentukan. Mereka khawatir risiko merusak koin langka dan mahal merupakan risiko yang terlalu besar untuk diambil.
1804 Bust Dollar – Class I (Dexter-Pogue Specimen)
Sekali lagi, “Raja Koin Amerika” mengambil salah satu dari 10 tempat teratas dalam daftar Koin Terlangka dan Paling Berharga di Dunia. Koin nya dilelang sebagai bagian dari D. Brent Pogue koleksi koin lelang bersama oleh Stack Bowers Galeri dan Sotheby selama rentang dua setengah tahun.
Spesimen ini memiliki huruf D kecil yang dilubangi awan di bagian belakang koin yang menunjukkan bahwa promenade itu milik James V. Dexter, seorang ahli numismatis kaya yang memilikinya selama 14 tahun pada akhir abad ke-19.
Seluruh koleksi menyadari $ 106,69 juta terjual di lima lelang terpisah. Ada 1804 dolar perak lainnya dalam koleksi koin Pogue (The Sultan of Muscat-Watters-Brand-Childs-Pogue) yang merupakan spesimen terbaik yang diketahui, tapi sayangnya, tawaran sebesar $ 10,81 juta tidak cukup tinggi untuk koin tersebut dijual. lelang 24 Mei 2016.
1804 Bust Dollar – Class I (Mickley-Hawn-Queller Specimen)
Ini adalah koin yang sama yang terdaftar sebagai #Koin Paling Berharga di Dunia di atas yang dijual seharga $ 3.737.500 pada bulan April 2008. Tidak seperti Nikel Kepala Liberty Five-O 1913 Hawaii yang kehilangan hampir $ 500.000 ketika dijual untuk kedua kalinya, ini pemilik mendapat keuntungan $ 140.000 saat dia menjualnya.
Hanya ada 15 spesimen asli yang diketahui dipukul pada tiga waktu berbeda. Dengan memeriksa koin dengan cermat, ahli numismatis profesional mengklasifikasikan masing-masing dari lima belas koin menjadi salah satu dari tiga klasifikasi: Kelas I atau “Asli,” Kelas II atau “Pemulihan Pertama” dan Kelas III atau “Pemulihan Kedua.”
Koin Kelas I memiliki populasi tertinggi dengan delapan koin yang diketahui ada. Kelas II adalah koin unik, dan Kelas III memiliki enam spesimen yang diketahui. Terlepas dari klasifikasinya, koin-koin ini selalu mencetak rekor ketika melewati blok lelang.
$1 Million Gold Canadian Maple Leaf
Pada tahun 2007, Royal Canadian Mint menghasilkan koin satu juta dolar pertama di dunia. Koin tersebut berukuran diameter 50 cm (20 inci) dengan tebal 3 cm (1,2 inci) dan berisi 100 kilogram (220 pound atau 3.215 troy ounce) dari 99,999% emas murni.
Ide untuk koin ini pada awalnya disusun sebagai inti untuk mempromosikan baris baru Royal Canadian Mint yang 99,999% murni satu koin emas Gold Maple Leaf Troy ons.
Hingga saat ini, lima dari koin emas batangan yang megah ini telah dibeli oleh investor dari seluruh dunia. Koin terakhir yang dijual di lelang publik dijual seharga 3,27 juta euro (USD 4,02 juta) di lelang di Wina di rumah lelang Dorotheum.
1804 Silver Dollar – Class I (The Watters-Childs Specimen)
Spesimen “King of US Coins” ini adalah contoh terbaik dari 1804 Silver Dollar dan dinilai Proof-68 oleh Professional Coin Grading Service. Ketika koin ini dijual pada Agustus 1999, itu menjadi koin paling berharga di dunia hingga saat ini. Ini dengan mudah mengalahkan pemegang rekor sebelumnya (1804 silver dollar “) dengan lebih dari dua kali lipat jumlah tersebut.

Beberapa pemilik sebelumnya termasuk: The Sultan of Muscat, CA Watters, Henry Chapman, Virgil Brand, Charles dan Ruth Green, Charles Frederick Childs dan Keluarga Pogue. Pada Mei 2016, 1804 Silver Dollar terbaik yang terkenal ini, yang awalnya dimiliki oleh Sultan Muscat pada tahun 1835 dan kemudian oleh Childs Family Collection selama lebih dari 50 tahun, sekali lagi dimasukkan ke dalam blok lelang oleh D. Brent Pogue.
Tawaran $ 10.575.000, yang paling banyak ditawarkan untuk koin, ditempatkan melalui telepon untuk 1804 Draped Bust Silver Dollar ini, tetapi gagal mencapai harga cadangan pengirim, rumah lelang Sotheby mengatakan dalam sebuah pernyataan.
10 Barang Antik Dan Koleksi Paling Berharga Sepanjang Masa – Dari satu hidangan China yang bernilai lebih dari $ 37 juta hingga umpan berburu langka yang masing-masing terjual lebih dari dua ratus ribu, bacalah tentang beberapa barang antik dan koleksi paling berharga yang memecahkan rekor yang pernah dijual di lelang.

Ru Guanyao Brush Washer Bowl
Piring kecil seperti ini yang digunakan untuk mencuci sikat kecil mungkin tidak terlihat banyak, tetapi memecahkan rekor dunia untuk porselen China pada tahun 2017. Dari Dinasti Song Utara, piring berusia 900 tahun yang berukuran hanya 5,125 inci ini terdaftar sebagai “sangat penting dan sangat langka “dalam katalog lelang. https://www.mustangcontracting.com/
“Barang-barang ‘Ru guanyao’ yang terkenal dengan lapisan biru kehijauan yang intens dan pola” keretakan es ” sangat langka karena kiln di provinsi Henan tengah China memiliki produksi singkat hanya sekitar dua dekade,” kata Reuters melaporkan penjualan.
Setelah pertarungan penawaran 20 menit, kapal kecil itu membawa setara dengan $ 37,68 juta dalam lelang Sotheby di Hong Kong. Ini memecahkan rekor sebelumnya yang dipegang oleh piala “ayam” yang terkenal pada tahun 2014.
Record-Breaking Persian Rug
Dengan perkiraan pra-lelang sebesar $ 5 hingga $ 7 juta, permadani antik ini jauh melebihi ekspektasi penjualan. Ini adalah salah satu karpet penting dari perkebunan William Andrews Clark yang dijual di lelang pada 2013. Harga palu akhir terakhir, termasuk premi pembeli, adalah jumlah yang luar biasa sebesar $ 33,76 juta.
Permadani itu dijelaskan oleh Sotheby sebagai berikut: Daun Sabit, gulungan sulur dan karpet teknik ‘Vas’ palmette, kemungkinan Kirman, Persia Tenggara. Kondisi dan kelangkaan berperan dalam membawa jumlah yang memecahkan rekor ini.
Patek Philippe Supercomplication Pocket Watch
Jam saku langka buatan Patek Philippe tahun 1932 ini memecahkan rekor dunianya sendiri. Dikenal sebagai Supercomplication Henry Graves Jr., ini dinamai “seorang bankir New York yang bersaing dengan pabrikan mobil James Ward Packard untuk mendapatkan jam tangan paling rumit di awal abad ke-20,” menurut Wall Street Journal.
Arloji saku dijual seharga $ 24 juta di lelang pada tahun 2014, memecahkan rekor sebelumnya set $ 11 juta pada tahun 1999 sebagai penunjuk waktu yang paling berharga dalam sejarah lelang.
Elizabeth Taylor’s La Peregrina Pearl Necklace by Cartier
Kalung mewah ini istimewa karena sejumlah alasan. Pertama, itu dibuat oleh Cartier, nama yang dikenal untuk menghasilkan beberapa perhiasan terbaik dan paling didambakan di dunia.
Maka Anda memiliki asalnya, karena dirancang untuk aktris Elizabeth Taylor untuk memegang perhiasan yang sangat istimewa: Mutiara La Peregrina abad ke-16 yang menakjubkan yang dibeli untuknya oleh Richard Burton pada tahun 1969.
Mengingat semua yang dimiliki perhiasan besar ini, tidak mengherankan jika Christie melaporkan bahwa ia menetapkan dua rekor lelang: satu untuk mutiara bersejarah dan satu lagi untuk permata mutiara menghasilkan $ 11.842.500 di lelang.
Robby the Robot Movie Prop
Dengan tinggi 7 kaki, prop film luar biasa ini (dijual bersama dengan Jeep futuristiknya) memecahkan rekor dunia sebagai yang termahal yang pernah dijual di lelang pada akhir 2017.
Robby the Robot, dari film fiksi ilmiah klasik, Planet Terlarang yang dirilis pada tahun 1956, dijual seharga $ 5,375 juta melalui Bonhams di New York. Ini memecahkan rekor sebelumnya untuk prop film non-otomotif yang sebelumnya dipegang oleh Maltese Falcon yang dijual seharga $ 4 juta pada tahun 2013, juga oleh Bonhams.
Honus Wagner Baseball Card
Kartu bisbol paling berharga sepanjang masa berasal dari awal 1900-an. Dengan hanya sembilan yang diketahui keberadaannya, contoh Honus Wagner dalam kondisi sangat baik seperti ini sangatlah langka dan berharga.
Contoh ini dijual seharga $ 3,12 juta pada tahun 2016, memecahkan rekor sebelumnya sebesar $ 2,8 juta yang dibuat dengan kartu Wagner yang berbeda pada tahun 2007. Perhatikan bahwa ada banyak reproduksi di pasar karena nilainya yang tinggi.
Dracula Record-Setting Movie Poster
Poster film Drakula tahun 1931 ini memecahkan rekor dunia termahal yang pernah dijual di lelang. Heritage Auctions menjual poster tersebut pada tahun 2017 seharga $ 525.800. Ini adalah salah satu dari dua contoh yang masih hidup yang diketahui.
Poster tersebut melampaui rekor lelang sebelumnya sebesar $ 478.000, yang juga ditetapkan (dua kali) oleh Heritage Auctions. Heritage baru saja menjual satu-satunya poster film terbitan Italia yang bertahan dari tahun 1946 untuk Casablanca pada Juli 2017, yang menyamai rekor dunia mereka sebelumnya dari November 2014 untuk salinan poster London After Midnight hanya diketahui tahun 1927″, menurut siaran pers Heritage Auctions.
Chippendale-Style Kentucky Desk
Paling sering ketika catatan furnitur antik dipecahkan, asal muasalnya adalah Rhode Island, New York, atau mungkin Pennsylvania. Namun pada akhir 2017, meja antik buatan Kentucky menjadi sorotan lelang.
Meja bergaya Chippendale yang diukir rumit yang terbuat dari kenari dibuat untuk Kapten John Cowan oleh pembuat yang tidak dikenal. Itu dijual seharga $ 498.750 harga tertinggi yang pernah dibayarkan di lelang untuk sebuah perabot Kentucky dan tertinggi kedua untuk perabot Southern, menurut sebuah laporan di Lexington Herald-Leader.
World Record Antique Doll
Pada Januari 2018, Rumah Lelang Theriault memecahkan rekor dunia, menjual boneka Prancis yang terkenal. Boneka antik pengaturan rekor diciptakan oleh Antoine Edmund Rochard. Itu dijual seharga $ 333.500, dan akan berada di Barry Art Museum of Norfolk, Virginia.
Menurut Theriault’s, pemimpin penjualan lelang boneka, contoh Rochard ini “melambangkan zaman keemasan boneka Prancis”. Itu juga menarik bagi para sarjana fotografi dan budaya dan sejarah Prancis karena pelindung dada boneka itu dihiasi dengan kalung yang dilukis dengan rumit.
Tersembunyi di dalam 24 permata kecil adalah foto mikro yang menggambarkan pemandangan bersejarah di Prancis, seperti Fontainebleau, Louvre, dan Hotel de Ville di Paris, antara lain. Saat dipegang erat ke mata, setiap gambar diperbesar 160 kali.

Carved Decoys by Important Makers
Sebagai bagian dari lelang umpan tersukses yang pernah diadakan, contoh yang ditunjukkan di sini memecahkan rekor tidak hanya untuk pemahat khusus ini, tetapi juga untuk pembuat umpan Kanada. Karya Thomas Carver ini dijual oleh Copley Fine Art Auctions, LLC seharga $ 270.000.
Dalam penjualan yang sama, sejumlah umpan lainnya memecahkan rekor pembuatnya, 19 di antaranya, termasuk drake pintail John English dan angsa Kanada Charles E. “Shang” Wheeler, masing-masing dijual seharga $ 246.000 dan $ 198.000.
Kamera Antik Yang Terbaik Untuk Dikoleksi – Berita yang sempat beredar bahwa Leica telah terjual di pelelangan dengan 72,4 juta pemecah rekor (sekitar £ 2,1 juta) mungkin membuat Anda berpikir Anda harus super kaya untuk membeli kamera vintage.
Tidak begitu. Ini adalah prototipe praproduksi yang sangat langka. Kembali di dunia nyata Anda dapat menemukan kamera film vintage yang sesuai dengan setiap saku, apakah Anda seorang kolektor, pengguna, atau sedikit dari keduanya. slot gacor
Kolektor membeli kamera untuk nilai historis atau fitur yang tidak biasa. Fotografer membeli kamera untuk memotret. Tapi ada tempat di mana kedua dunia bertemu. Berikut adalah pilihan jenis kamera vintage terjangkau yang dikumpulkan oleh pengumpul dan pengguna. americandreamdrivein.com
1. Exakta Varex IIb

– Diluncurkan 1963
– Harga panduan £ 30- £ 40
Mungkin Anda suka ide refleks lensa tunggal (SLR) 35mm. Ada banyak Prakticas dan Zenits sekitar kurang dari £ 50, tetapi bagaimana dengan nama yang lebih bergengsi seperti Exakta ini? Ini olahraga lensa Domiplan 50mm f / 2.8, dipertukarkan dengan berbagai panjang fokus yang berbeda.
Asesoris termasuk penglihatan mata setinggi mata atau setinggi pinggang. Kamera juga berbagi fitur yang menarik dengan Exaktas lain: kemampuan untuk memasangkan panggil kecepatan rana dengan kontrol tindakan yang tertunda untuk menghasilkan kecepatan lambat hingga 12 detik.
2. Kodak Retina II
– Diluncurkan 1936
– Harga panduan £ 35 – £ 45
Ketika Kodak memperkenalkan Retina pada tahun 1934, itu membuat fotografi 35mm yang mahal lebih terjangkau bagi massa. Pada saat Retina II diluncurkan dua tahun kemudian, itu telah berkembang menjadi kamera 35mm berkualitas yang dilipat menjadi paket berukuran saku dan berdiri tegak melawan orang-orang seperti Leica dan Contax.
Ada beberapa variasi. Yang ini adalah Tipe 142, dengan pengintai yang digabungkan, lensa Kodak Ektar 5cm f / 3.5 yang fokus dari 3,5 kaki hingga tak terbatas dan rana Compur-Rapid berkecepatan 1-1 / 500detik.
3. FED dan Zorki
– Diluncurkan 1934 dan 1948
– Harga panduan £ 25 – £ 40
Apakah Anda suka Leica? Sayangnya, Anda tidak akan menemukan satu di bawah £ 50, tetapi Anda dapat membeli salinan Fed Rusia atau Zorki Leica yang terjangkau. Ketika Leitz memperkenalkan Leica, ia gagal mematenkan desain di Rusia, karenanya kamera FED dan Zorki, yang secara legal dibuat salinannya.
Masing-masing terlihat dan beroperasi seperti Leica II dengan spesifikasi serupa: daun jendela fokus, pengukur jarak dekat, lensa f / 3.5 dan kecepatan rana 1 / 20-1 / 500sec. Secara mekanis dan optikal mereka mungkin tidak memenuhi standar tinggi dari aslinya Jerman, tetapi mereka biasanya dapat diandalkan dan lensa mereka memiliki reputasi untuk kualitas.
4. Zeiss Box Tengor
– Diluncurkan 1934
– Harga panduan £ 10 – £ 15
Kamera kotak dulunya adalah favorit keluarga. Anda dapat mengambil satu untuk kurang dari satu pon di pameran boot. Tetapi jika Anda menginginkan sesuatu dengan lebih dari spesifikasi dasar, lihat kisaran Box Tengor yang dibuat oleh Zeiss Ikon. Model 54/2 ini memiliki lensa Goerz Frontar f / 11 pemfokusan, kecepatan rana tetap, dan tiga lubang yang dapat disesuaikan, dan dibutuhkan gambar 6x9cm besar pada 120 film.
5. Seagull 4B
– Diluncurkan 1972
– Harga panduan £ 85 – £ 95
Pikirkan refleks lensa kembar (TLR) dan pikiran beralih ke Rolleiflex yang mahal. Bahkan Rolleicord, versi Rolleiflex yang dipreteli, masih mendapat banyak uang saat ini. Tapi Rolleicord disalin oleh produsen di seluruh dunia, dan salinan itu jauh lebih terjangkau. Versi ini berasal dari Cina.
Ini adalah TLR tradisional yang bagus dengan lensa kembar untuk memotret dan melihat, layar pemfokusan 6x6cm besar di atas bodi untuk mencocokkan ukuran gambar pada 120 rollfilm, lensa pengambilan 75mm f / 3.5 dan rana 1–1 / 300detik kisaran kecepatan.
6. Kiev 6C

– Diluncurkan 1980
– Harga panduan £ 70- £ 90
Pindah ke kisaran harga ini dan Anda dapat membeli refleks rollfilm format menengah seperti Kiev buatan Rusia. Besar, berat, dan merekam eksposur 12 6x6cm pada 120 rollfilm, atau 24 eksposur pada 220 film. Biasanya ditemukan dengan jendela bidik setinggi pinggang, penambahan jendela bidik TTL memberikan pengukuran mata melalui lensa.
Lensa standar Vega 90mm f / 2.8 dikenal karena ketajamannya, dan kamera menerima lensa aksesori melalui dudukan yang dibagikan dengan Pentacon Six. Rilis rana kiri sedikit canggung dan getaran dari tamparan cermin besar berarti paling baik digunakan pada tripod saat memotret di bawah 1/112 detik.
7. Foca PF3
– Diluncurkan 1955
– Harga panduan £ 75 – £ 90
Kamera pengintai antik 35mm dilambangkan oleh pabrikan Jerman atau Jepang. Tetapi Prancis juga aktif di bidang ini, terutama dengan kamera Foca. Ini adalah Foca PF3 (PF singkatan dari Petit Format).
Meskipun bukan salinan Leica yang sebenarnya, ini menunjukkan pengaruh Leica, dengan lensa Oplar 5cm f / 3.5 yang memanjang dari tubuh untuk pemotretan, panggilan cepat yang dipasang di atas dari 1 / 25-1 / 1000sec dan panggilan cepat yang terpisah untuk 1 -1 / 25sec di bagian depan.
8. Praktina IIA
– Diluncurkan 1958
– Harga panduan £ 60 – £ 80
Nikon F, diluncurkan pada tahun 1959, umumnya diakui sebagai sistem 35mm SLR pertama. Tetapi tiga tahun sebelumnya, FX Praktina Jerman Timur diluncurkan sebagai bagian dari sistem besar, dan itu ditingkatkan menjadi Praktina IIA setahun sebelum Nikon F tiba.
Kamera berada di tengah-tengah berbagai macam aksesori yang mencakup pengukur ketinggian pandang setinggi pinggang, setinggi mata, dan tinggi; perangkat close-up; layar fokus yang dapat diganti; penggerak motor listrik dan jarum jam; lampiran stereo dan belakang film besar yang menampung 17m film. Itu terlihat di sini dengan jendela bidik pentaprismenya yang terukur dan lensa standar Carl Zeiss Jena Flexon 50mm f/2.
9. Contax IIIa
– Diluncurkan 1951
– Harga panduan £ 200 – £ 220
Sebelum Perang Dunia Kedua, Zeiss Ikon membuat Contax I, II dan III di Dresden. Setelah perang, perusahaan berpisah dan produksi dilanjutkan di Stuttgart, di mana kamera diluncurkan kembali sebagai Contax IIa dan IIIa. IIIa adalah yang terbaik dari lima. Meter selenium yang dipasang di atas memberikan bacaan yang diatur secara manual.
Pemfokusan dilakukan dengan menggunakan thumbwheel kecil yang menonjol dari pelat atas dan ada pengintai yang digabungkan untuk memastikan akurasi. Lensa Sonnar pasca-perang biasanya ditemukan dengan kamera luar biasa.
10. Robot II
– Diluncurkan 1939
– Harga panduan £ 100 – £ 150
Pada tahun 1934, Robot I membawa drive motor jarum jam bawaan ke kamera 35mm. Model pertama itu adalah tengara yang menarik minat kolektor, tetapi kaset film non-standar membuatnya sulit digunakan saat ini. Model kedua mengambil kaset 35mm normal, menghasilkan lebih dari 50 eksposur 24x24mm dalam satu roll.
Motor terluka oleh kenop besar di pelat atas, setelah itu film secara otomatis berliku setelah setiap paparan. Itu membuatnya bagus untuk fotografi candid, yang selanjutnya dibantu oleh viewfinder yang dapat dialihkan untuk digunakan pada 90 ° ke subjek. Berbagai lensa termasuk nama Tessar yang bergengsi.
Berbagai Alat Musik Tertua Yang Ada di Dunia – Musik sering disebut bahasa universal dunia. Tidak masalah dari mana pun berasal, semua orang tampaknya memahami perasaan yang ditimbulkan oleh musik. Meskipun kita mungkin tidak pernah tahu pasti kapan nenek moyang kita pertama kali mengembangkan musik, kita tahu bahwa beberapa contoh awal alat musik muncul lebih dari 40.000 tahun yang lalu.
Temuan ini menunjukkan bahwa manusia modern awal yang pertama kali bermukim di Eropa sudah memiliki tradisi musik, diyakini bahwa mereka menciptakan instrumen mereka segera setelah mereka menetap di Eropa. idn slot
Nenek moyang kita mungkin telah mengembangkan musik sekitar 50.000 tahun yang lalu, selama “ledakan budaya”, periode ketika manusia mulai menciptakan seni, perhiasan, dan menguburkan orang mati secara seremonial. https://americandreamdrivein.com/
1. Seruling Geisenklösterle

– Usia: 42.000 – 43.000 tahun
– Negara Asal: Gua Geisenklösterle, Blaubeuren, Jerman
– Bahan yang Digunakan: Mute Swan bone dan Mammoth Ivory
Tiga seruling yang ditemukan di situs arkeologi Gua Geisenklösterle adalah instrumen tertua di dunia. Dua seruling terbuat dari tulang angsa bisu dan seruling lainnya terbuat dari gading mammoth.
Para peneliti memiliki radio karbon tanggal seruling dan memperkirakan bahwa mereka berusia antara 42.000 dan 43.000 tahun. Seruling dihubungkan dengan Aurignacian, budaya arkeologis yang terkait dengan manusia modern paling awal di Eropa.
Beberapa peneliti percaya bahwa seruling ini, dan alat musik awal lainnya, membantu kelompok besar manusia purba mengembangkan dan mempertahankan ikatan yang kuat. Mereka percaya bahwa ikatan ini membantu spesies kita memperluas wilayahnya lebih jauh daripada Neanderthal yang lebih konservatif, yang punah di sebagian besar Eropa sekitar 30.000 tahun yang lalu.
2. Divje Babe Flute
– Usia: 43.100 tahun
– Negara Asal: Cerkno, Slovenia
– Bahan yang Digunakan: Gua Beruang Femur
Sebelum ditemukan seruling tulang yang lebih tua, Divje Babe Flute dianggap sebagai contoh tertua dari alat musik yang pernah ditemukan di dunia. Selama bertahun-tahun seruling telah menarik pendapat yang berbeda tentang siapa yang membuat seruling dan apakah itu benar-benar objek buatan manusia atau tidak.
Beberapa arkeolog percaya bahwa seruling itu dibuat oleh Neanderthal sementara yang lain menyatakan bahwa seruling itu dibuat oleh Cro-Magnons.
Pada 2015, sebuah penelitian baru dirilis yang menyatakan bahwa seruling itu sebenarnya hanya tulang yang dikunyah oleh hyena. Jika temuan dalam penelitian ini benar, sekarang tidak ada bukti yang ada bahwa Neanderthal memiliki pengetahuan untuk membuat alat musik. Meskipun temuan baru, seruling saat ini ditampilkan di Museum Nasional Slovenia sebagai seruling Neanderthal.
3. Hohle Fels Flute
– Usia: 35.000 – 40.000 tahun
– Negara Asal: Gua Hohle Fels, Baden-Württemberg, Jerman
– Bahan yang Digunakan: Griffon Vulture Bone
Seruling dari gua Hohle Fels ditemukan pada musim gugur 2008 dan berusia antara 35.000 hingga 40.000 tahun. Dari semua seruling tulang kuno yang ditemukan sejauh ini, yang dari Hohle Fels adalah yang paling lengkap dan sangat mirip dengan seruling modern. Instrumen ini sekitar 8,5 inci panjangnya dan bagian dari instrumen di mana musisi meniup masih dalam kebijaksanaan.
Para arkeolog mengatakan bahwa seruling ini dan yang lainnya ditemukan di wilayah tersebut “menunjukkan keberadaan tradisi musik yang mapan pada saat manusia modern menjajah Eropa.” Beberapa tahun yang lalu, Wulf Hein, seorang “arkeolog eksperimental”, membuat replika seruling dan menggunakannya untuk memainkan The Star-Spangled Banner.
4. Isturitz Flutes
– Usia: 20.000 – 35.000 tahun
– Negara Asal: Gua Isturitz, Prancis
– Bahan yang Digunakan: Vulture Wing Bones
Seruling yang ditemukan di situs arkeologi Isturitz di barat daya Prancis berusia sekitar 20.000 hingga 35.000 tahun. Fragmen dari lebih dari 20 seruling terpisah ditemukan di lokasi. Seruling dibuat oleh berbagai budaya yang hidup di daerah tersebut termasuk Aurignacian, Gravettian, dan Magdalenian.
Sementara sebagian besar seruling itu berkeping-keping, dua seruling paling lengkap diciptakan oleh budaya Gravettian dan berusia antara 22.000 dan 28.000 tahun. Seruling ini dibuat dengan baik dan menunjukkan tanda-tanda penggunaan yang jelas, terutama di sekitar lubang jari. Area di sekitar lubang jari terlihat dipoles, yang telah diartikan sebagai keausan saat bermain.
5. Bullroarer

– Usia: sekitar 20.000 tahun
– Negara Asal: Berbagai belahan dunia; contoh tertua dari Ukraina dan Perancis
– Bahan yang Digunakan: Bilah tipis dari kayu dan kabelnya
Bullroarer adalah alat musik ritual yang digunakan oleh banyak budaya kuno dan saat ini di seluruh dunia. Secara historis, itu digunakan untuk berkomunikasi jarak jauh. Contoh tertua dari bulroarer yang ditemukan di Ukraina, berasal dari periode Paleolitik (sekitar 18.000 SM). Selain bulroarer tertua dari Ukraina, para arkeolog telah menemukan bullroarer kuno di bagian lain Eropa, Asia, Afrika, anak benua India, Australia, dan Amerika.
Meskipun beberapa budaya telah menggunakan bulroarer, Aborigin Australia terkenal karena menggunakan instrumen tersebut. Suku Aborigin menggunakan bulldoger dalam upacara inisiasi, pemakaman untuk mengusir roh jahat, dan melawan pertanda buruk.
6. Lithophones
– Usia: berusia antara 4.000 dan 10.000 tahun
– Negara Asal: Berbagai belahan dunia; contoh tertua dari India dan Vietnam
– Bahan yang digunakan: Batuan resonansi
Nama “lithophone” digunakan untuk alat musik apa pun yang terbuat dari batu yang menghasilkan nada musik ketika dipukul. Jenis instrumen kuno ini telah ditemukan di seluruh dunia, dengan beberapa contoh tertua yang diketahui berasal dari Vietnam.
Lithophones dari Vietnam disebut Dan Da dan terdiri dari 11 lempengan batu besar, diposisikan secara vertikal dekat satu sama lain. Para peneliti menentukan bahwa batu-batu itu dipahat dan dapat menghasilkan musik dengan memukulnya.
Salah satu contoh lithophones yang paling terkenal adalah Musical Stones of Skiddaw. Lebih dari dua abad, serangkaian litofon dibangun di sekitar kota Keswick di Inggris utara.
7. Jiahu Flutes
– Usia: 7.000 – 9.000 tahun
– Negara Asal: Jiahu, Lembah Sungai Kuning, Cina
– Bahan yang digunakan: Tulang sayap Red-Crown Crane
Seruling tulang yang ditemukan di situs arkeologi Jiahu adalah alat musik tertua yang diketahui dari Tiongkok. Tiga puluh tiga seruling di berbagai negara bagian ditemukan di lokasi – sekitar 20 seruling utuh dan sisanya rusak atau terfragmentasi.
Enam dari seruling lengkap dan dianggap sebagai alat musik multinote tertua yang dapat dimainkan yang pernah ditemukan. Ukuran seruling bervariasi dan memiliki lima, enam, tujuh, atau delapan lubang.
Para peneliti telah memainkan seruling paling awet dan telah mengunggah rekaman audio yang menampilkan tanda-tanda musik yang berusia ribuan tahun. Analisis nada mengungkapkan bahwa seruling tujuh-lubang menghasilkan nada yang mirip dengan skala delapan nada Barat yang akrab yang dimulai dengan “do, re, mi.”
8. Trumpet Tutankhamun
– Usia: sekitar 3.340 tahun
– Negara Asal: Mesir
– Bahan yang digunakan: Satu dengan perak murni, yang lain dari perunggu atau tembaga
Sepasang trompet dari makam Firaun Tutankhamun diyakini sebagai trompet yang dapat dimainkan tertua di dunia. Sangkakala ini adalah satu-satunya yang selamat dari Mesir kuno dan berusia lebih dari 3.000 tahun.
Mereka ditemukan pada tahun 1922 oleh arkeolog Howard Carter selama penggalian makam Tutankhamun. Kedua fitur terompet itu diukir dengan indah dengan gambar dekoratif dewa Ra-Horakhty, Ptah, dan Amun.
Pada tahun 1939, trompet dimainkan sebelum audiensi langsung dan pertunjukannya disiarkan secara internasional melalui radio BBC. Sejak penemuan mereka, ada klaim bahwa trompet memiliki kekuatan untuk memanggil perang. Orang-orang menghubungkan Inggris memasuki Perang Dunia II dengan terompet karena perang di Eropa dimulai lima bulan setelah siaran BBC.
Barang Koleksi dan Barang Antik Paling Berharga Sepanjang Masa – Dari salah satu penawaran barang antik di Cina yang bernilai lebih sebesar $ 37 juta hingga sebuah umpan berburu langka yang masing-masing terjual lebih dari dua ratus ribu, oleh karena itu, simaklah tentang berbagai macam barang antik dan koleksi yang paling berharga serta memecahkan rekor yang pernah dijual di lelang.
1. Ru Guanyao Brush Washer Bowl

Sebuah piring kecil seperti ini yang digunakan untuk mencuci sikat kecil mungkin tidak terlihat seperti banyak, tetapi itu menetapkan rekor dunia untuk porselen Cina pada tahun 2017. Dari Dinasti Song Utara, hidangan berusia 900 tahun ini yang berukuran hanya 5,125 inci terdaftar sebagai “sangat penting dan sangat jarang “dalam katalog lelang. raja slot
“Barang-barang ‘Ru guanyao’ seperti itu – dikenal dengan glasir biru-hijau yang intens dan pola” keretakan es “- sangat jarang karena kiln di provinsi Henan pusat China hanya memiliki produksi singkat sekitar dua dekade,” kata Reuters. laporan penjualan. www.americannamedaycalendar.com
Setelah pertempuran penawaran dalam waktu 20 menit, kapal kecil ini pun membawa setara dengan $ 37,68 juta dalam pelelangan Sotheby di Hong Kong. Ini memecahkan rekor sebelumnya yang dipegang oleh piala “ayam” yang terkenal pada tahun 2014.
2. Record-Breaking Persian Rug
Dengan perkiraan dalam pra-lelang $ 5 hingga $ 7 juta, karpet antik ini jauh melebihi harapan penjualan. Ini adalah salah satu karpet penting dari tanah William Andrews Clark yang dijual di lelang pada 2013. Harga palu-turun terakhir, termasuk premi pembeli, adalah jumlah luar biasa $ 33,76 juta.
Karpet itu yang diuraikan oleh Sotheby sebagai berikut: sebuah Sickle-Leaf, gulungan anggur dan karpet ‘Vase’-teknik palmette, mungkin Kirman, Persia Tenggara. Kondisi serta kelangkaan yang memainkan peran dalam membawa jumlah pemecahan rekor ini.
3. Patek Philippe Supercomplication Pocket Watch
Arloji saku langka yang dibuat oleh Patek Philippe pada tahun 1932 ini memecahkan rekor dunianya sendiri. Dikenal sebagai Supercomplication Henry Graves Jr., dinamai setelah “seorang bankir New York yang bersaing dengan produsen mobil James Ward Packard untuk menugaskan arloji yang paling rumit mungkin pada awal abad ke-20,” menurut Wall Street Journal.
Arloji saku dijual seharga $ 24 juta di lelang pada tahun 2014, memecahkan rekor sebelumnya sebesar $ 11 juta yang ditetapkan pada tahun 1999 sebagai arloji paling berharga dalam sejarah lelang.
4. Elizabeth Taylor’s La Peregrina Pearl Necklace by Cartier
Kalung mewah ini khusus untuk sejumlah alasan. Pertama, itu dibuat oleh Cartier, nama yang dikenal untuk memproduksi beberapa perhiasan terbaik dan paling didambakan di dunia. Maka Anda memiliki asalnya, karena itu dirancang untuk aktris Elizabeth Taylor untuk memegang perhiasan yang sangat istimewa: La Peregrina Pearl abad ke-16 yang menakjubkan dibeli untuknya oleh Richard Burton pada tahun 1969.
Dengan semua yang telah dilakukan oleh perhiasan besar ini, tidak mengherankan bahwa Christie melaporkan bahwa ia membuat dua catatan lelang: satu untuk mutiara bersejarah dan satu lagi untuk permata mutiara — membawa $ 11.842.500 di lelang.
5. Robby the Robot Movie Prop
Berukuran 7 kaki, prop film yang luar biasa ini (dijual bersama dengan Jeep futuristiknya) memecahkan rekor dunia sebagai yang termahal yang pernah dijual di lelang pada akhir 2017.
Robby the Robot, dari film fiksi ilmiah klasik Forbidden Planet yang dirilis pada tahun 1956, dijual dengan harga $ 5,375 juta melalui Bonham di New York. Ini menghancurkan rekor sebelumnya untuk film prop non-otomotif yang sebelumnya dipegang oleh Maltese Falcon yang dijual seharga $ 4 juta pada 2013, juga oleh Bonhams.
6. Honus Wagner Baseball Card
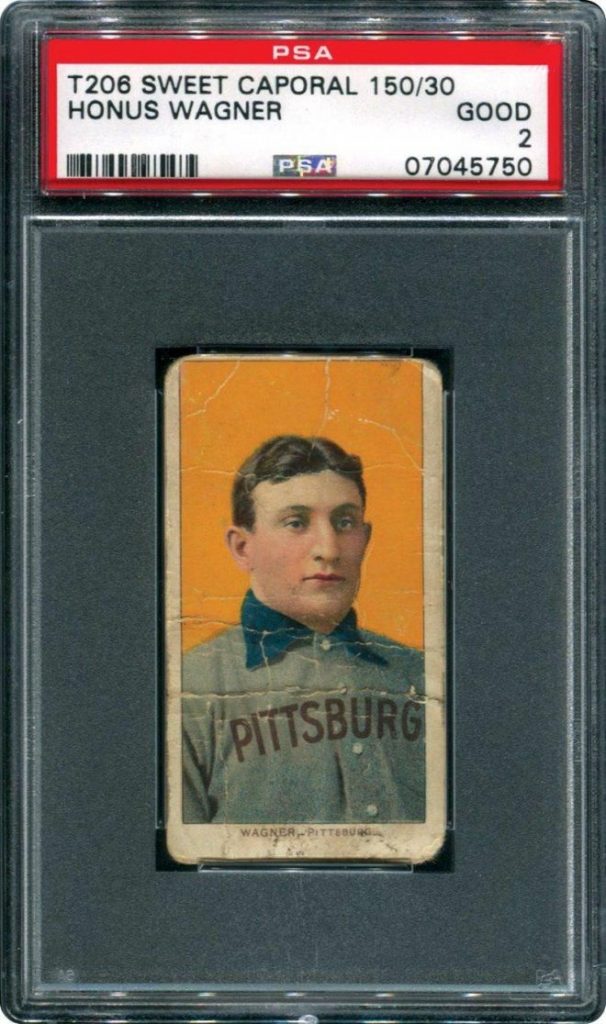
Kartu baseball yang begitu berharga sepanjang masa hingga awal 1900-an. Dengan cuma sembilan yang diketahui ada, contoh Honus Wagner dalam kondisi sangat baik seperti ini sangat langka dan berharga.
Contoh ini dijual seharga $ 3,12 juta pada tahun 2016, memecahkan rekor sebelumnya sebesar $ 2,8 juta yang ditetapkan dengan kartu Wagner yang berbeda pada tahun 2007. Perhatikan bahwa ada banyak reproduksi di pasar karena nilainya yang tinggi.
7. Dracula Record-Setting Movie Poster
Poster film Dracula ini dari tahun 1931 memecahkan rekor dunia untuk yang paling mahal yang pernah dijual di lelang. Heritage Auctions menjual poster pada 2017 dengan harga $ 525.800. Ini adalah satu dari dua contoh yang masih ada yang diketahui.
“Poster itu melampaui rekor lelang sebelumnya sebesar $ 478.000, yang juga ditetapkan (dua kali) oleh Heritage Auctions. Heritage baru saja menjual satu-satunya poster film Italia yang masih hidup yang diketahui dari tahun 1946 untuk Casablanca pada Juli 2017, yang cocok dengan rekor dunia sebelumnya dari November 2014 untuk salinan poster yang hanya diketahui untuk London After Midnight 1927, “menurut untuk siaran pers Lelang Warisan Budaya.
8. Chippendale-Style Kentucky Desk
Paling sering ketika catatan mebel antik rusak, asal potongan adalah Rhode Island, New York, atau mungkin Pennsylvania. Namun pada akhir 2017, sebuah meja antik buatan Kentucky menjadi sorotan lelang.
Meja gaya Chippendale yang diukir rumit yang terbuat dari buah kenari dibangun untuk Kapten John Cowan oleh pembuat yang tidak dikenal. Itu dijual seharga $ 498.750 – harga tertinggi yang pernah dibayarkan di lelang untuk sepotong furnitur Kentucky dan tertinggi kedua untuk sepotong furnitur Selatan, menurut sebuah laporan di Lexington Herald-Leader.
9. World Record Antique Doll
Pada Januari 2018, Rumah Lelang Theriault memecahkan rekor dunia, menjual boneka Prancis terkenal. Boneka antik pengaturan rekor diciptakan oleh Antoine Edmund Rochard. Itu dijual seharga $ 333.500, dan akan tinggal di Barry Art Museum of Norfolk, Virginia.
Menurut Theriault’s, pemimpin dalam penjualan lelang boneka, contoh Rochard ini “melambangkan masa keemasan boneka Prancis.” Ini juga menarik bagi para sarjana fotografi dan budaya Prancis serta sejarah karena tutup dada boneka itu dihiasi dengan kalung yang dilukis dengan rumit.
Tersembunyi di dalam 24 permata kecil adalah foto mikro yang menggambarkan pemandangan bersejarah di Prancis, seperti Fontainebleau, Louvre, dan Hotel de Ville di Paris. Pada saat dipegang erat pada mata, setiap gambar diperbesar 160 kali.
10. Carved Decoys by Important Makers
Sebagai bagian dari lelang umpan paling sukses yang pernah diadakan, contoh yang ditampilkan di sini memecahkan rekor tidak hanya untuk pemahat khusus ini, tetapi untuk pembuat umpan Kanada. Karya Thomas Carver ini dijual oleh Copley Fine Art Auctions, LLC dengan harga $ 270.000.
Dalam penjualan yang sama, sejumlah umpan lainnya memecahkan rekor untuk pembuatnya, 19 di antaranya, termasuk drake pintail John English dan angsa Charles E. “Shang” Wheeler Canada, masing-masing dijual seharga $ 246.000 dan $ 198.000.
Daftar Berbagai Mobil – Mobil Vintage Terbaik – Di setiap era, perusahaan manufaktur mobil yang berbeda telah memperkenalkan model terbaru mereka untuk pecinta mobil dan untuk bersaing dengan saingan mereka. Demikian pula, setiap era memiliki beberapa model mobil kelas atas yang membedakan pabrikan mereka di antara para pesaing karena fitur dan spek yang unik.
Industri mobil telah menjadi satu-satunya industri yang telah tumbuh bahkan selama masa perang dan resesi ekonomi. Selama seratus tahun terakhir telah ada banyak mobil klasik top yang telah memenangkan hati jutaan pecinta mobil. Namun, hanya beberapa mobil klasik yang bisa mengalahkan yang lain dalam hal kinerja, gaya dan pengalaman berkendara secara keseluruhan. dewa slot
Di sini kita melihat sekilas daftar mobil-mobil klasik dan mobil-mobil top yang telah memenangkan hati banyak orang dan terus melakukan hal yang sama hari ini. https://www.americannamedaycalendar.com/
1. 1969 MASERATI GHIBLI 4.7

Nama Maserati menghasilkan banyak pengaruh dan merupakan salah satu mobil klasik terbaik yang menggunakan bingkai tubular dengan tubuh terpisah. Suspensi depan menggunakan tipe double wishbone, coaxial damper dan coil spring, dan anti-roll bar.
Di bagian belakang terdapat beberapa fitur luar biasa yang mencakup lengan torsi tunggal memanjang dengan gandar hidup pada pegas semi-eliptik, peredam hidrolik, dan bar anti-roll. Juga, roda magnesium adalah standar. Sedangkan Maserati melengkapi mobil dengan dua tangki bahan bakar 50 L independen, yang dapat diisi melalui flap.
2. 1957 MERCEDES 300SL GULLWING
Pintu-pintu dari Mercedes membuatnya menjadi salah satu mobil paling keren dan klasik sepanjang masa. Fakta bahwa 300SL adalah mobil produksi tercepat pada saat itu, yang tidak berlebihan.
Mercedes-Benz 300 SL adalah mobil klasik paling autentik untuk dipugar yang diproduksi oleh Mercedes-Benz. Ini memiliki injeksi bahan bakar langsung mekanis, meningkatkan kekuatan hampir 50%. Oleh karena itu, ia mampu mencapai kecepatan tertinggi hingga 263 km / jam serta mobil produksi tercepat pada masanya.
3. 1960-JAGUAR E-TYPE
Jaguar E-type diperkenalkan oleh Pasar Amerika Utara dan disebut “mobil paling indah yang pernah dibuat” oleh Enzo Ferrari. Jaguar E-Type mengklaim kecepatan tertinggi 150 mph dan akselerasi 0 hingga 60 mph. Ini juga memiliki konstruksi monocoque serta rem cakram. Ia juga memiliki plus rack-and-pinion plus, suspensi depan dan belakang independen
4. 1966 SHELBY 427 COBRA
Apa pun yang terlampir pada nama Carroll Shelby segera bernilai waktu Anda dan merupakan mobil klasik terbaik untuk dibeli. Plus, kobra menggabungkan mesin Ford V-8 dan ringan tubuh AC Ace Inggris untuk membuat beberapa mobil Amerika paling liar dan paling dicari. Top-line V-8 427-cubic-inch Cobra dikombinasikan dengan dua supercharger Paxton, memberikan kekuatan ganda daripada yang lain.
5. 1958 CHEVROLET IMPALA
Tidak ada mobil lain yang dapat mengalahkan Chevrolet Impala 1958 dalam hal desain, gaya, dan kinerja dan oleh karena itu pasti mengambil tempat nomor satu pasti. Hingga saat ini, mobil ini sangat diminati oleh para kolektor dan bahkan oleh mereka yang suka mengendarai mobil klasik.
Karenanya, sudah pasti menjadi yang pertama dalam daftar mobil klasik. Chevrolet Impala memiliki opsi mesin berbeda untuk pembeli yang dapat menghasilkan 234 tenaga kuda. Sirip besar juga menjadi faktor gaya khas orang kaya dan terkenal.
6. FORD MUSTANG 1967
Dianggap sebagai mobil berotot terbaik pada masa itu, Ford Mustang 1967 jelas merupakan yang teratas dalam daftar mobil klasik. Desain keseluruhan mobil hanya elegan dan tidak peduli bagaimana Anda mengendarainya, mobil ini tidak akan mengecewakan Anda. Ford Mustang adalah kombinasi gaya dan kekuatan dan karena itu ia menerima respons yang fenomenal.
Mesin Big Block yang ditambahkan ke dalamnya adalah binatang dari keindahan ini dan dapat dengan mudah mengalahkan sebagian besar mobil-mobil vintage di era yang sama.
7. 1969 CORVETTE STING RAY

Ini jelas merupakan mobil ikonik dan Anda dapat mengetahuinya dari desain mobil. Ini adalah salah satu mobil klasik yang dirancang terbaik dan karena itu orang masih mencari keindahan ini sehingga mereka dapat membelinya dan menyimpannya. Sting Ray 1969 coupe adalah sesuatu yang bisa membuat Anda tergoda karena memiliki penampilan dan faktor kinerja yang digabungkan bersama. Ini memiliki suspensi belakang split, rem cakram, mesin blok besar, jendela belakang split dan pipa knalpot samping. Mobil ini sangat populer dan karenanya Anda akan melihatnya di berbagai film Hollywood juga.
8. 1948 TUCKER
Apakah Anda suka membuat orang menoleh saat berkendara di jalan? Ya, itulah yang bisa dilakukan 1948 oleh Tucker. Mobil adalah karya seni dan inovasi dan masih tetap menjadi salah satu mobil yang paling dicari.
Dirancang oleh Preston Tucker dan Alex Tremulis 1948 Tucker sulit ditemukan dan oleh karena itu faktor harga untuk mobil ini akan tinggi walaupun Anda menemukannya. Mobil ini tidak dibuat dalam banyak dan karena itu Anda hanya akan menemukan orang-orang selektif memiliki Tucker 1948 dan menikmati fitur-fitur inovatif yang keluar dari dunia pada saat itu. Salah satu Mobil Klasik yang langka
9. 1964 PORSCHE 911
The 911 oleh Porsche masih sangat laris tetapi 1964 Porsche 911 adalah sesuatu yang harus Anda miliki jika Anda tergila-gila pada mobil klasik Anda. Ketika mobil diluncurkan pada tahun 1964, mobil ini memiliki pendingin udara yang dipasang di belakang mesin dan transmisi manual lima kecepatan.
Meskipun dibuat untuk 4 penumpang, kursi belakang tidak nyaman tetapi mobil ini menyenangkan bagi pengemudi.
10. 1953 ASTON MARTIN DB2
Aston Martin adalah salah satu produsen mobil top di dunia dan pada tahun 1953 mereka datang dengan DB2 yang tetap menjadi salah satu mobil klasik top yang pernah dibuat. Mobil ini memiliki mesin overhead cam ganda 6 yang lebih besar yang dirancang untuk memberikan kinerja lebih.
Mesin akan menambah tenaga kuda ke kinerja dan karena itu itu adalah mobil terbaik yang pembalap akan lebih suka pada saat itu. Namun, mobil tetap dalam produksi hanya selama 3 tahun dan oleh karena itu hanya model terbatas yang tersedia saat ini.
11. 1962 MASERATI 3500
The 1962 Maserati 3500 Classic Cars hampir seperti penemuan kembali model 1957 tetapi perusahaan telah mengalami perubahan yang berbeda untuk memastikan bahwa mobil tidak hanya mampu tampil lebih baik tetapi juga terlihat hebat.
Maserati 3500 1962 memiliki lebih banyak fitur seperti power window, tempat duduk kulit, rem cakram, mesin enam silinder dan transmisi empat kecepatan yang akan membutuhkan kecepatan.
12. 1967 VOLKSWAGEN BEETLE
Beetle jelas merupakan salah satu mobil berdesain terbaik di dunia karena masih memegang perhatian pembeli & pecinta mobil klasik. Namun, itu Beetle 1967 yang memiliki banyak perbaikan yang membuat mobil klasik ini lebih populer daripada versi lainnya.
Ini memiliki drive train baru dan mesin dan generator listrik yang luar biasa. Itu sarat dengan fitur yang akan membuat mengemudi lebih baik untuk pengemudi dan menambah performa mobil. lihat di film Hollywood The Love Bug, juga
Barang Antik Unik Yang Bisa Membuat Anda Mendapatkan Uang Tambahan – Anda mungkin akan sangat terkejut dengan sejumlah benda sehari-hari yang mungkin Anda miliki atau Anda lihat di sekitar rumah Anda, yang bisa bernilai dengan jumlah besar uang. Bisa jadi hal-hal yang Anda mungkin tidak pernah dianggap berharga. Mari kita periksa bagaimana Anda bisa mengetahui apakah Anda memiliki barang kolektor di rumah Anda. Mari cari tahu di mana tempat terbaik untuk menilai mereka. Anda dapat menghasilkan uang mudah yang dapat menghemat Anda harus mengambil pinjaman jangka pendek cepat di masa depan.
Siapa sangka, bertahun-tahun yang lalu, bahwa barang-barang kolektor yang khas seperti perangko, koin, dan kartu telepon BT tidak akan sepopuler atau seproti kaset video langka atau album vinil? Lukisan 70 jelek yang dilemparkan ke loteng, atau patung keramik yang dulunya milik nenek Anda sekarang bisa bernilai besar! Dari barang-barang pribadi hingga pusaka keluarga, hal-hal yang dapat ditemukan di sekitar rumah atau di dalam kotak di loteng atau garasi dapat bernilai uang. Terlebih lagi dengan barang-barang yang langka atau persediaan terbatas. Anda tidak hanya dapat menjual barang-barang antik yang berharga ini untuk banyak uang tunai, Anda juga dapat menggunakannya sebagai jaminan jika Anda ingin mengambil pinjaman yang dijamin dari pegadaian. nexus slot
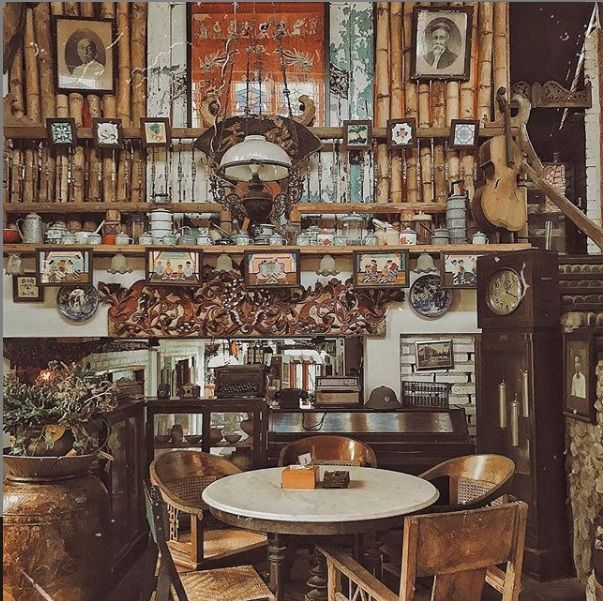
Kolektor barang antik
Apakah orang benar-benar siap untuk membayar barang langka semacam ini?
Memang benar. Anda akan kagum pada hal-hal yang orang siap membayar uangnya. Orang-orang akan membeli barang antik koleksi yang dapat memberi mereka hubungan emosional dengan masa kecil mereka. Ini bisa berupa mainan, kaset video favorit, dan gadget pertama yang mereka miliki. Barang-barang antik yang bisa dikoleksi ini dapat memunculkan perasaan bahagia yang menghubungkannya dengan waktu dan tempat tertentu ketika semuanya baik. Orang lain membeli barang yang menghubungkan mereka dengan orang yang dicintai atau anggota keluarga. Banyak orang akan membeli barang-barang antik yang bisa dikoleksi yang membawa mereka banyak sukacita sebagai anak-anak dan membayar ratusan untuk melihat mereka dikembalikan ke kejayaan mereka. www.mrchensjackson.com
Berikut adalah beberapa contoh cara menemukan barang berharga yang mungkin ada di rumah Anda.
1. Uang menghasilkan Uang

Koin selalu menjadi barang kolektor favorit. Jangan khawatir jika Anda tidak memiliki koleksi koin bagus yang diwariskan kepada Anda sebagai pusaka keluarga. Koin modern, yang mungkin Anda miliki dalam bentuk uang saku, bisa bernilai banyak uang. Sudah waktunya untuk memeriksa kapal pengumpul koin yang mungkin Anda dan keluarga Anda miliki di rumah untuk menemukan harta karun tersembunyi di depan mata.
Royal Mint kadang-kadang membuat kesalahan pada koin yang dicetak dan mungkin perlu beberapa waktu sebelum kesalahan ini ditemukan dan diperbaiki. Baru-baru ini, koin 50p langka telah berpindah tangan untuk beberapa ratus pound. Kew Gardens, Olimpiade dan peringatan 50p EC, sepotong 20p tanpa tanggal dan 2p dicetak dengan “Pence Baru” dari tahun 1983 adalah semua koin yang harus diperhatikan.
2. Catatan Vinyl
Rekaman vinil bisa menjadi salah satu hal paling mahal di rumah Anda. Sebagian besar dari kita menyingkirkan koleksi rekaman vinil kami dan bergegas untuk merangkul teknologi kembali di tahun delapan puluhan ketika CD menjadi cara baru untuk mendengarkan musik. Hari ini piringan hitam membuat kembali besar. Banyak artis berkinerja merilis album baru mereka di vinil serta dengan cara biasa. Catatan vinil yang paling berharga adalah berpindah tangan untuk jumlah uang yang sangat banyak. Anda dapat memeriksa daftar online untuk beberapa yang paling populer. Pemutar rekaman keluarga juga bisa bernilai besar bagi seseorang yang menginginkan pemain serupa memainkan vinyl mereka.
3. Mainan kuno
Periksa rumah Anda untuk mainan vintage yang berharga. Mainan vintage dapat dijual dengan untung besar jika dikemas dan dalam kondisi baik, tetapi mainan bekas yang masih sangat dicintai masih dicari. Set Lego sangat populer dengan set yang terjual hingga beberapa kali harga pembelian aslinya. Mobil adalah barang kolektor lain yang populer, terutama Hot Wheels dan mainan Tonka. Boneka koleksi porselen, terutama boneka Amerika masa awal, dapat dijual dengan harga tinggi seperti halnya boneka Sindy, boneka Barbie, dan mainan Star Wars, apa pun kondisinya.
4. Set teh dan ruang makan

Teh dan perangkat makan dapat menjadi beberapa barang paling mahal yang Anda miliki. Peralatan keluarga biasanya tidak digunakan dan diturunkan dari generasi ke generasi. Beberapa barang antik yang bisa dikoleksi ini bisa bernilai uang yang mengejutkan. Penting bahwa tidak ada kerusakan dan set sudah selesai. Barang-barang semacam ini adalah contoh klasik dari sesuatu yang mungkin tidak berguna bagi Anda, dikemas dalam sebuah kotak di loteng. Namun, itu bisa memberi Anda uang tambahan dan menghindari Anda tidak harus mengambil pinjaman penjamin dan juga dapat dinikmati oleh seseorang yang akan menggunakannya.
5. Keramik dan perak
Silverware selalu ditandai dengan jelas memungkinkan Anda untuk melihat pembuatnya, usia dan di mana ia diproduksi. Meskipun tidak terlalu populer saat ini, perak masih dapat dijual karena nilainya dalam berat untuk membawa beberapa pound ekstra. Keramik dari nilai apa pun memiliki stempel yang jelas pada pangkalan yang memungkinkan Anda untuk dengan mudah memeriksa online dan mencari tahu kapan dan di mana mereka dibuat dan nilai apa yang mereka miliki. Barang dagangan Royal Dalton, Royal Worcester, dan Staffordshire semuanya pantas untuk dikunjungi.
6. Mebel dan perlengkapan lampu
Bukan hanya barang antik koleksi dari abad sebelumnya yang berharga. Dengan barang-barang Art Deco menjadi sangat populer di desain rumah, sebuah meja tua atau lampu dari tahun 20-an atau 30-an bisa sangat berharga tanpa Anda sadari. Mebel Ikea tua dari tahun 70-an dijual hingga sepuluh kali lipat dari harga yang dibayarkan ketika awalnya dibeli. Banyak dari barang-barang ini yang tidak populer pada saat itu yang diproduksi yang menyebabkan garis jatuh dan tidak banyak yang dibuat, yang membuatnya langka dan dicari hari ini.
7. Buku dan komik
Komik-komik kuno yang semula dibeli dengan harga beberapa pence bisa bernilai puluhan ribu poundsterling, bahkan jutaan dalam kasus komik Superman edisi pertama. Komik yang biasanya lebih bernilai adalah komik tempat pahlawan baru atau penjahat diperkenalkan, terutama mereka yang terkenal dalam film aksi hari ini yang membuatnya lebih relevan bagi banyak kolektor. Bukan hanya buku-buku antik yang bisa memberi Anda uang, beberapa buku masa kecil yang mungkin Anda miliki termasuk The Wind in the Willows, Charlotte’s Web, dan The Secret Garden semuanya sangat bisa dikoleksi. Buku-buku Harry Potter dapat menghasilkan banyak uang dan tidak harus dalam kondisi bersih. Savethestudent adalah situs yang bagus untuk membantu Anda mengetahui berapa banyak yang dapat Anda peroleh dari barang-barang lama Anda.
Inilah Merek Berbagai Sepeda Motor Vintage – Beberapa cerita yang pasti membuat marah untuk setidaknya beberapa orang, dan ini mungkin salah satunya.
Koleksi Sepeda Motor
Pemilik, pengendara, dan pengoleksi sepeda motor tua begitu bersemangat sehingga menyoroti satu merek atau model sepeda motor yang lain pasti akan mendapat reaksi keras.
Memang, sulit untuk memikirkan tato merek nama pelanggan di tubuh mereka lebih dari Harley-Davidson. slot
Baik itu Harley atau Honda atau India, terdapat gairah yang kuat dan mengikuti yang mendorong mereka yang mampu membayar lebih dari $ 1 juta-plus untuk sepeda motor vintage yang sangat didambakan, meskipun juga mungkin untuk mengambil satu untuk hanya $ 100. https://www.mrchensjackson.com/
Penting untuk diingat bahwa sepeda motor vintage belum tentu dapat dikoleksi, itu juga bisa berarti bahwa itu sudah tua.
Tidak ada definisi yang diterima secara luas untuk berapa usia sepeda motor harus memenuhi syarat sebagai vintage, tetapi beberapa ahli mengatakan itu sesuatu yang lebih tua dari 1974, dan yang lain benjolan di sepeda Jepang dari awal 1980-an. idn play

Menurut John Cerilli, salah satu pendiri Vintage Motorcycles Online, untuk menjadi vintage dan tertagih adalah fungsi dari sejumlah faktor, termasuk kondisi dan keaslian sepeda motor,
kapan dan berapa banyak sepeda dibuat, berapa lama perusahaan yang membuatnya dalam bisnis dan apakah sepeda dikaitkan dengan seseorang yang terkenal.
Baca terus untuk mengetahui beberapa merek sepeda motor vintage paling populer di luar sana hari ini.

1. Brough Superior
Orang sering kagum pada bagaimana biaya sepeda motor vintage dapat meroket selama bertahun-tahun, membuat mereka cukup berharga sehingga beberapa investor menggunakannya untuk menyeimbangkan portofolio saham dan obligasi mereka. Namun, beberapa sepeda mahal sejak awal.
Beberapa atasan Brough, yang dibuat oleh perusahaan yang didirikan oleh George Brough, menelan biaya sebanyak rumah pada saat mereka dibebaskan. Jelas, sepeda mendapatkan julukan mereka sebagai “The Rolls Royce of Motorcycles,” yang merujuk tidak hanya pada harga tinggi mereka, tetapi juga fakta bahwa Brough hanya menggunakan bahan terbaik untuk merakit motornya.
Selanjutnya
Belakangan ini, banyak orang mengasosiasikan Brough Atasan dengan TE Lawrence, lebih dikenal sebagai Lawrence of Arabia. Untuk sedikitnya, Lawrence adalah pengendara Brough yang setia, memiliki total delapan, masing-masing memiliki nama:
Yang pertama disebut Boa, sedangkan sisanya bernama George I, George II dan seterusnya dan seterusnya, hingga George VII, sepeda yang dia tunggangi ketika dia meninggal – George VIII dalam pesanan, tetapi tidak pernah dikirimkan.
2. Kawasaki
Ada argumen yang dibuat bahwa perusahaan yang berspesialisasi, baik itu di widget atau ponsel atau sepeda motor, akan memiliki fokus yang diperlukan untuk menghasilkan produk yang unggul untuk bisnis yang melakukan sedikit dari segalanya.
Perusahaan Jepang Kawasaki, yang mulai membuat sepeda motor pada 1960-an, dapat membantah teori itu, mengingat bahwa ia memiliki warisan pembuatan kapal, jet dan peralatan industri sebelum memasuki bisnis roda dua.
Bahkan, ketika datang ke beberapa model vintage Kawasaki yang paling terkenal, tampak jelas bahwa perusahaan itu bersemangat untuk memberikan apa yang ia tahu tentang membuat mesin besar yang kuat untuk kerajinan pembuatan sepeda motor, terutama tenaga tinggi 1969 500 cc Mach III dan 1973 900 cc 4 silinder Z1. Z1,
khususnya, dianggap oleh beberapa orang sebagai “sepeda super” pertama di zaman modern. Itu bisa berjalan sangat cepat (antara 120 mph dan 130 mph) seperti Corvette atau Ferrari, tetapi harganya jauh lebih murah.

3. Vincent-HRD
Jauh sebelum The Beatles mendarat di pantai Amerika Serikat dan memulai era musik yang ditentukan oleh band-band Inggris, sejumlah perusahaan sepeda motor AS membuat sepeda sangat dicari di Amerika.
Di antara perusahaan yang lebih terkenal yang melihat keberhasilan mengekspor barang-barang mereka ke Amerika adalah Vincent, yang didirikan oleh Philip Conrad Vincent. Menurut Cerilli dari Vintage Motorcycles Online, Vincent mulai merancang suspensi belakang yang inovatif saat ia belajar teknik mesin di Cambridge, desain yang ia masukkan ke dalam sepeda motor Vincent pertamanya.
Saat ini, Vincent Black Shadow adalah sepeda motor yang sangat berharga, dengan harga antara $ 75.000 dan lebih dari $ 250.000, karena hanya 1.700 yang dibuat dan karena fitur yang dibanggakannya ketika pertama kali dirilis.
Contoh
Misalnya, Wagnon dari Motorcycle Mechanics Institute mengatakan bahwa Vincent Black Shadow 1948 mungkin adalah sepeda motor yang diproduksi secara massal tercepat pada masanya.
“Ini benar-benar 100 mil per jam sepeda motor dalam waktu 60 mil per jam sepeda. Mereka cepat dan kuat dan maju untuk waktu mereka,” kata Wagnon. “Setiap kolektor vintage, termasuk saya, akan senang memiliki Vincent.”
4. Moto Guzzi
Merayakan ulang tahunnya yang ke-90 pada tahun 2011, menjadikannya sebagai produsen sepeda motor yang terus beroperasi terpanjang kedua, Moto Guzzi memulai karirnya di tepi Danau Como di Lombardy, Italia ketika co-founder Carlo Guzzi tidak dapat menemukan motor yang sempurna dan malah memutuskan untuk membangun itu sendiri.
Dikenal sebagai “Elang” Italia yang hebat, Moto Guzzi telah membedakan dirinya sebagai pembangun sepeda motor yang memenangkan balapan;
Bahkan, perusahaan memperkirakan sepeda telah membawa pulang sekitar 3.300 judul selama sejarahnya. Beberapa model vintage perusahaan yang lebih terkenal termasuk Le Mans, Falcone dan El Dorado, yang dibedakan berdasarkan gaya dan keandalannya.
Mungkin sejarah yang paling menarik di sekitar motor Moto Guzzi adalah dari V7 Sport asli, yang telah dihidupkan kembali dan dimodifikasi hari ini menjadi V7 Café Classic. Pada 1960-an dan 70-an, V7 Sports diidentifikasi dengan kelompok tandingan yang dikenal sebagai Rocker.
Dimulai di Inggris dan kemudian menyebar ke Eropa dan Amerika, V7 Sports digunakan dalam perlombaan di mana pesaing akan mulai di sebuah kafe dan berusaha untuk mencapai titik yang telah ditentukan dan kemudian kembali sebelum lagu di jukebox selesai.
5. BMW
Dikenal sebagai “sepeda motor pria yang berpikir” karena tekniknya yang elegan dan perawatannya yang sederhana, BMW telah membuat sejumlah motor yang oleh banyak ahli vintage dianggap sebagai signifikan. Menurut Nolan Woodbury, salah satu pendiri Vintage Motorcycles Online,
pabrikan Jerman yang dihormati mungkin harus berterima kasih kepada Honda karena telah mendorongnya untuk memproduksi beberapa sepeda vintage terbaiknya, terutama 1973 R90S dan R100RS. “Melebihi dari semuanya, R90S adalah bukti bahwa BMW mengakui Jepang sebagai ancaman terhadap pangsa pasar mereka,” katanya.
Perilisan
Sebelum perilisan Honda CB750 1969, Woodbury mengatakan bahwa BMW tidak peduli dengan penawarannya, lebih atau kurang memberitahu pelanggannya yang kaya untuk mengambil atau meninggalkan sepeda hitam mereka dengan sepeda bergaris-garis putih atau pergi mencari sesuatu yang lain.
CB750
Semua itu berubah ketika CB750 Honda tiba di lokasi. “Asap yang abu-abu atau oranye mencolok R90S diperkenalkan untuk membuktikan BMW adalah hip untuk generasi baru pengendara sepeda motor dan disetel sehingga mengungguli CB750. R100RS adalah kelanjutan dari tema ini,
lebih mewah dan tidak seperti apa pun yang ditawarkan Jepang, untuk sementara waktu, ” dia berkata.
Berbagai Sepeda Antik Yang Paling Dikoleksi – Sepeda antik adalah investasi unik. Sepeda begitu menarik sehingga membuat senang dari para penggemar sepeda dan sekarang maju berpikir investor karena mereka tidak kehilangan nilainya dari waktu ke waktu, tetapi hanya meningkatkan nilainya tahun ke tahun.
Seringkali, banyak sepeda langka hanya diproduksi selama satu tahun dan dikendarai oleh legenda bersepeda, mereka sedikit dan jarang dan sejarah mereka jauh lebih menarik daripada pasar saham.
Di Steel Vintage Bikes kami cukup beruntung telah disemarakkan oleh banyak sepeda paling langka dan paling dihargai di dunia. Oleh karena itu, kami berikan kepada Anda 10 sepeda paling dapat dikoleksi di Steel Vintage Bikes … Sedikit pengetahuan orang dalam yang ingin kami bagikan dengan Anda! slot online
1) Bianchi Centenario 1985

Bagaimana cara merayakan 100 tahun dalam bisnis? Buatlah sepeda yang sangat tampan dan keren, tanpa kesulitan. Selamat datang di Bianchi Centenario. Dapat dikenali secara instan, ikon dalam warna dan gaya. Setiap bagian dari sepeda ini diberi pantographed dengan ‘Bianchi Centenario’, hanya untuk menjadikannya istimewa. www.benchwarmerscoffee.com
Frame adalah jantung dari setiap Bianchi dan ini tidak terkecuali. Ini memiliki tabung Colombus SLX yang diwarnai dengan lembut dengan cat krommeto gunmetal khusus. Namun tidak berhenti sampai di situ, Bianchi bekerja lebih keras dan melengkapi Centenario dengan groupset Campagnolo C-Record dan hub jalan bintang sheriff yang sangat langka!
Estetika motor ini sangat lembut di mata dan pengerjaan membuat sepeda tahan uji waktu. Ini adalah salah satu keindahan langka dan setiap tahun mereka semakin sulit ditemukan.
2) Colnago Arabesque
Ulang tahun lagi, kelangkaan lain. Satu untuk para kolektor, Colnago Arabesque diproduksi untuk menghormati ulang tahun ke-30 Colnago dan hanya berada di jalur manufaktur antara tahun 1983 dan 1984. Bicylce Colnago paling lengkap yang pernah diproduksi, dalam jumlah terbatas dijual dengan Campagnolo Super Record Gruppo.
Gruppo ini menggabungkan 7/8 klub Colnago emas dan kerangka Arabes memiliki dua klub emas lebih lanjut dimasukkan ke dalam topi seatstay. Namun, ini sangat sulit ditemukan.
‘Lugs’ memberi Colnago tampilan yang sangat berbeda dan frameset dibentuk untuk memaksimalkan keuntungan dari kualitas berkendara baja. Ini menghasilkan perjalanan yang tak terlupakan dengan sepeda paling sederhana yang paling indah. Benar, hanya masalah menemukan satu sekarang.
3) Wilier Triestina Ramata
Menarik, elegan, diinginkan, tertagih dan tentu saja langka: Wilier Triestina Ramata. Berasal dari Italia, rumah manufaktur ini didirikan pada tahun 1906 oleh Pietro Dal Molin, di sepanjang tepi sungai Brenta di Bassano Del Grappa.
Ramata diterjemahkan menjadi dilapisi tembaga dan inilah yang memberikan frame sepeda ini hasil akhir yang berbeda. Lihat saja, benar-benar sempurna, jika Anda melihatnya, Anda bahkan dapat melihat bayangan Anda sendiri. Ini adalah merek dagang Wilier Triestina dan jika sepeda ini dapat digunakan, Bassano Del Grappa pasti patut dikunjungi.
4) Bianchi Tour de France 1953
Ketika kita memikirkan celeste, kita memikirkan Bianchi. Ketika kita memikirkan Bianchi Tour De France 1953, kita memikirkan Fausto Coppi. Setelah kekacauan kehilangan saudaranya pada tahun 1952, ia bangkit lagi dengan gaya yang penuh teka-teki, menenangkan para penentang dan bersepeda ke buku-buku sejarah dengan menyapu ganda Giro de Italia dan Tour de France.
Untuk menghormati kemenangan yang tak tertandingi, Bianchi memproduksi crème de la crème, Tour de France.
Apa yang benar-benar memisahkan sepeda ini dari yang lain adalah ia membuka jalan bagi masa depan bersepeda. Itu adalah salah satu sepeda pertama yang cocok dengan rantai ganda standar dan memiliki kabel deraille Campagnolo dioperasikan pertama.
Selain itu, salah satu dari banyak faktor yang menyebabkan sepeda ini begitu langka adalah hanya diproduksi selama satu tahun. Karena cara kemenangan Coppi, model dan nama diubah untuk mencerminkan hal ini.
Terobosan dalam pengerjaan, sepeda ini mewujudkan sifat pahlawannya; Fausto Coppi.
5) Colnago Oval Cx

Status kultus untuk Colnago sudah tercapai pada saat Oval Cx keluar, jadi ke mana Anda pergi dari sana? Aerodinamika adalah jawaban Colnago. Usaha Colnago ke dalam efek aerodinamis pra-tanggal pengembangan dan penggunaan teknik-teknik tersebut oleh tim bersepeda AS pada tahun 1984.
Colnago sudah tertelungkup di terowongan angin tahun sebelumnya meneliti setiap elemen terakhir untuk menciptakan sepeda yang sempurna. Tubing ovalisasi membahas masalah kekakuan bingkai, semua kabel dirutekan secara internal dan rem roda belakang dipasang di dalam bingkai untuk menawarkan daya tahan yang lebih kecil terhadap angin. Ringan, cepat dan sulit ditemukan, kami tidak akan memiliki cara lain di Steel Vintage Bikes.
6) Casati Gold Line
Membangun bingkai adalah seni dan Casati telah menyempurnakan permainan mereka selama lebih dari 90 tahun. Yang ini untuk kolektor, mereka yang suka mengendarai sepeda dan mengenal sepeda, Anda mungkin tidak melewati garis finish terlebih dahulu, tetapi Anda pasti akan jatuh cinta pada sepeda ini.
Dirancang dan direkayasa di bengkel Moza mereka di Italia, Casati Gold Line adalah model top of range. Pengerjaan sangat indah. Gold Line terbuat dari tabung Columbus SLX dengan rincian tambahan, seperti chainstays dengan ribbing khas Casati, jembatan rem dan lug dengan ukiran Casati. Tentu saja, sentuhan akhir adalah garpu berlapis emas asli dan chainstays.
Beruntung bagi Anda, SVB memiliki mahakarya sepeda yang menunggu untuk pergi ke rumah baru. Jika perhatian pada detail, pengerjaan yang sangat baik dan halus adalah apa yang Anda cari di dalam sepeda, maka Casati Gold Line cocok untuk Anda.
7) Rigi Bici CORTA
Sepeda itu terlalu menarik bagi Giorgio Rinaldi, yang meninggalkan kariernya sebagai desainer furnitur untuk mengembangkan dan menyempurnakan pengerjaan dengan sepeda. Diterjemahkan secara harfiah ke ‘Rigi Short Bike’,
Rinaldi melempar konvensi ke luar jendela dan secara drastis mengubah konfigurasi tabung kursi menggunakan dua tabung yang lebih kecil, alih-alih tabung kursi standar berdiameter 1 “. Ini memungkinkan segitiga belakang menjadi jauh lebih pendek, menempatkan roda belakang di antara tabung kursi kembar.
Ini berdampak pada pengendara dengan memungkinkan mereka untuk memiliki kontrol lebih, menjadi benar-benar terjalin dengan sepeda. Tabung kembar ditempatkan di tepi luar cangkang bb memberikan struktur kaku yang tidak ada duanya.
Sepeda ini benar-benar menjadi hidup di tanjakan bukit dan berlari, meninggalkan sisanya di jejak debu. Cahaya kuning dan hijau yang cerah dari sepeda menjadi spek di cakrawala, karena kami mempertanyakan diri kami sendiri karena tidak membeli sepeda yang dirancang sedemikian indahnya.
8) Frejus 1949
Didirikan di Turin pada tahun 1896 oleh Emmo Ghelfi, Frejus akan segera memantapkan dirinya di antara pabrikan bersepeda terkenal. Pembalap juara termasuk Cino Cinelli, Guiseppe Olmo dan bahkan Gino Bartali. Frame Frejus ramping, halus dan biasanya selesai dengan beberapa pekerjaan lug yang menyenangkan. Mereka memiliki gaya yang mudah, tidak keras atau sunyi tetapi jelas menonjol dari kerumunan.
Buatan tangan dan hanya dilengkapi dengan komponen-komponen terbaik pada masanya, orang Italia tampaknya hanya menyukai sepeda. Ini melambangkan bersepeda vintage.
Sulit untuk memilih apakah akan menggantung sepeda ini dari tembok atau untuk menemukan jalan terbuka terdekat dan hanya menghidupkan kembali balap tahun 1940-an. Di SVB jalan terbuka akan terlalu banyak godaan dengan sepeda ini!
Review: Destinasi Barang Antik Yang Unik di Eropa – Pada musim gugur tahun lalu, saya merasa senang karena bepergian ke Inggris bersama Toma Clark Haines, seorang pemandu barang antik veteran dan pemilik perusahaan wisata barang antik terbesar di Eropa, The Antiques Diva.
Pandangan Tentang Dunia Barang Antik
Pengalaman itu benar-benar mengubah pandangan saya tentang dunia barang antik, dan apa yang ditawarkannya. Itu juga memperkuat cinta saya kepada orang-orang yang terlibat. premium303
Mencari harta yang sempurna itu bisa membawa Anda ke sudut toko atau ke tujuan yang jauh yang menurut Anda sudah Anda ketahui, tetapi Anda sadar bahwa Anda tidak melakukannya. Pengalaman-pengalaman ini akan menuntun Anda untuk belajar, mencintai, dan bernafsu terhadap hal-hal yang tidak pernah Anda sadari sebelumnya. https://www.benchwarmerscoffee.com/
Di bawah ini adalah tiga tujuan barang antik terbaik dan menawan yang kami kunjungi, dan tiga sekarang kami memiliki saran dari Diva sendiri kami akan sangat merekomendasikan tur. Saya pasti akan. Maukah kamu?
1. Lorfords Antiques di Tetbury, The Cotswolds

Sebuah kota legendaris dengan sejarah setingkat tokoh-tokoh sastra, London tidak kekurangan toko barang antik yang indah. Dari Pimlico Road ke Kensington’s Church Street, mereka berlimpah. Tetapi meskipun ada undian yang jelas untuk barang antik kota Charles Dickens wax sarkastik tentang,
tahun-tahun terakhir telah melihat perubahan mendasar dari jalur pemburu harta ini menuju sebuah kota kecil di The Cotswolds dengan nama Tetbury. Dulunya merupakan situs benteng bukit kuno, sekarang Tetbury terkenal dengan keanggunan arsitekturnya, keindahan alamnya, dan lebih dari dua puluh toko barang antik semuanya berjalan kaki satu sama lain.
Yang paling dipuji dari gerombolan itu, Lorfords, duduk di pusat kota dan membawa semuanya mulai dari Georgia, ke Gustavian, hingga perabot dan aksesoris dekoratif abad pertengahan di garasi bus yang dikonversi dengan apik. Rekan pemilik, Toby Lorford dan Lesley Ferguson, mengandalkan selera mereka yang sempurna untuk melengkapi ruangan.
“Ini bukan ruang sakral,” kata Lorford, “kami akan selalu memilih sesuatu yang benar-benar ajaib atau berbicara khusus kepada kami untuk ditampilkan.” Dan menurut pendapatnya, Anda juga harus! “Jika Anda membeli sesuai selera Anda, hampir semua hal akan berjalan bersama,” katanya.
Sebagian Besar
Dengan sebagian besar karya menampilkan elemen tujuan, keanggunan, proporsi, gaya, keindahan, dan penyelesaian sulit untuk meninggalkan dengan tangan kosong. Pemandu barang antik veteran Toma Clark Haines, setuju: “Anda akan menemukan 1% teratas dari Pasar Loak Paris di Lorfords.” Lorford dengan tepat mengakui,
“Dengan semua toko di sini plus The Hangars proyek terbaru kami yang berlokasi di dekatnya yang menampung hampir empat puluh dealer – Anda tidak akan menemukan pilihan barang antik Tetbury di mana pun di Inggris di luar pasar malam utama.”
2. The Hangar at Babdown Airfield di Tetbury, The Cotswolds
Ketika datang ke antiquing, adakah yang lebih menarik dari sensasi perburuan? Tanyai para genius di balik toko Lorfords yang terkenal di Tetbury! Pada 2014, tim perintis di Lorfords memulai proses mengubah dua gantungan pesawat era WW2 di Babdown Airfield menjadi salah satu tujuan barang antik paling tak terduga di Eropa.
Hari ini, Hangar One dan Hangar Two house yang tepat bernama kira-kira 40 dealer barang antik yang dipilih dengan cermat (dengan skor lebih banyak duduk cantik di daftar tunggu)! Setiap dealer menampilkan campuran furnitur dan barang antik abad pertengahan yang dikuratori yang mencakup berbagai gaya dan periode.
Sementara Hangar pasti menggelitik indera romansa dan petualangan kami, mereka juga menawarkan layanan yang benar-benar luar biasa dengan pilihan luar biasa. Di mana lagi Anda dapat mengalami kemudahan gabungan dan rentang belanja online dengan layanan yang Anda dapatkan dari toko dealer tunggal?
Dan sementara masing-masing hanggar memiliki anggota penjualan khusus yang dapat membantu Anda menemukan bagian yang Anda inginkan di situs, keduanya juga lebih dari senang untuk menyampaikan berita di antara pemasok dealer jika potongan langka atau tidak biasa itu berada di luar jangkauan Anda.
Saran Bijak
Seperti saran bijak, Toby Lorford adalah di antara favorit kami: “Jangan terpaku pada periode, gaya, atau orisinalitas: Anda hanya harus fokus pada perabotan rumah Anda dengan hal-hal yang membuat Anda bahagia.
Dan jika Anda merasa kewalahan, duduklah, minum kopi dan ingat apa yang Anda sukai! Tidak ada aturan untuk perabotan rumah Anda. ” Benar dia. Antiquing tentu bukan lagi olahraga nenek Anda. Bawa kamu ke lapangan terbang!
3. Tur Pasar Loak Paris Dengan The Antiques Diva

Marché aux Puces de Saint-Ouen Paris, atau Pasar Loak Paris, adalah barang legenda. Asal-usulnya menelusuri kembali ke akhir abad ke-19 ketika karakter kain dan tulang berkumpul di dekat pelabuhan kota untuk menjual furnitur yang penuh kutu dan banyak lagi.
Saat ini, strukturnya bersifat permanen dan untungnya kutu tidak lagi menjadi masalah kesulitan sebenarnya terletak pada dengan sigapnya manuver 14 bagian yang tersebar lebih dari 750.000 kaki persegi dari apa yang dianggap sebagai pasar barang antik terbesar di dunia. Semuanya, mulai dari furnitur Louis XVI Empire hingga desain Art Deco dan seni suku berbaris di labirin lorong-lorong dan kios-kios penuh desain.
Herein memasuki perusahaan tur barang antik terbesar dan paling terkenal di Eropa, The Antiques Diva & Co. Perusahaan ini berspesialisasi dalam membantu Anda menghindari jebakan pembeli barang antik pemula dan berpengalaman.
Pemandu lokal akan menjemput Anda di hotel dengan tur yang disesuaikan dengan kebutuhan Anda. Panduan ini juga akan berfungsi sebagai penerjemah, menegosiasikan harga, dan bekerja sama dengan pengirim nasional untuk memastikan pembelian Anda aman di rumah. Masih agak waspada?
Pemandu Tur Barang Antik
Perusahaan ini dinobatkan sebagai satu-satunya Pemandu Tur Barang Antik Paul Bert Serpette yang disetujui pasar andalan Pasar Loak Paris dan salah satu yang paling terkenal. Toma Clark Haines, pemilik The Antiques Diva, mengatakan, ”Ini adalah salah satu tempat terbaik di dunia untuk berbelanja jika Anda tahu ke mana harus pergi.
Penjual kami mengenal kami, dan ketika kami masuk kami diberikan harga sebenarnya, bukan harga turis. ” Pada akhirnya, ia menggemakan sentimen banyak orang di industri barang antik: “Beli apa yang Anda sukai.”
4. Venesia, Italia Tur bersama The Antiques Diva
Ketika seseorang berpikir tentang Venesia, barang antik mungkin bukan yang pertama kali terlintas dalam pikiran. Sebagai gantinya, gambar-gambar piazza dan jembatan, jalanan berbatu-batu, Basilika San Marco, kaca Venesia, kanal dan gondola, dan gairah di atas segalanya tampak besar.
Tetapi kota Italia di dunia lain di Laut Adriatik ini adalah rumah bagi palazzo bersejarah dan toko-toko tersembunyi yang penuh dengan harta, meskipun seperti yang diketahui oleh siapa pun yang telah mengunjungi kota yang mempesona ini, sama frustasinya dengan menarik. Ada dua wajah Venesia:
Satu terlihat oleh turis dan yang lainnya terbuka untuk penduduk setempat dan teman-teman mereka. Di sinilah The Antiques Diva & Co. masuk. Pemandu lokal akan membawa Anda melalui jaringan kanal, lorong, jembatan, dan pulau labirin dan memperkenalkan Anda ke dealer yang tidak akan pernah Anda temukan sendiri. Ini adalah Venesia yang benar-benar baru, dan di mana pesona pengalamannya benar-benar tidak hilang.
The Antiques Diva sendiri, Toma Clark Haines, menggambarkan bagian dari tur: “Gambar duduk di Grand Canal di gondola, berbelanja di palazzo. Itu masih salah satu pengalaman paling romantis dan nyata dalam hidup saya. Saya harus mencubit diri sendiri setiap kali saya di sana.
Lukisan Berkualitas
” Selain romansa, Venesia adalah pusat banyak gerakan artistik dan budaya, khususnya selama periode Renaissance. Karenanya, lukisan berkualitas museum berlimpah dan untuk harga yang layak mempertimbangkan nilainya.
Kota ini juga merupakan rumah bagi berbagai macam patung antik yang menginspirasi dan tempat penyimpanan yang dijelaskan oleh Clark Haines sebagai “fenomenal.” Dan sementara kita tidak akan mengharapkan sesuatu yang kurang dari tempat kelahiran komposer Baroque yang terkenal, Antonio Lucio Vivaldi, ornamen dan kerawang dalam musik tercermin dalam perhiasan.